Coverage Determination Form
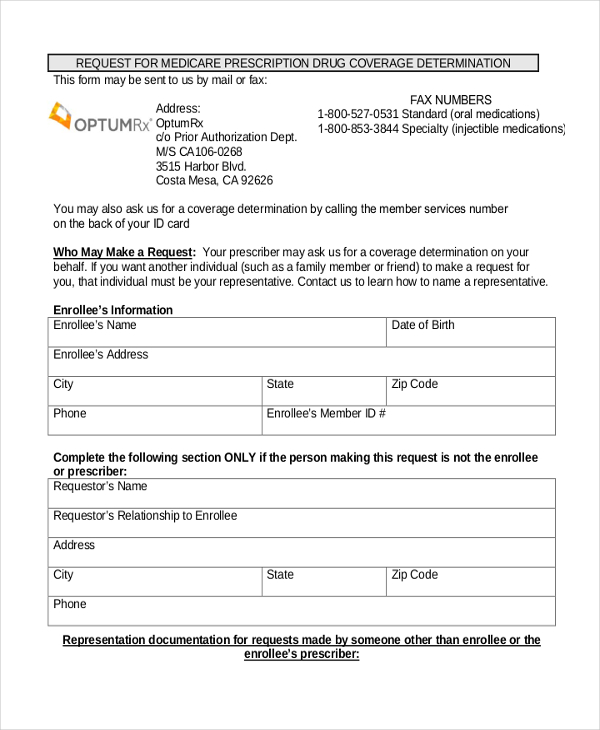
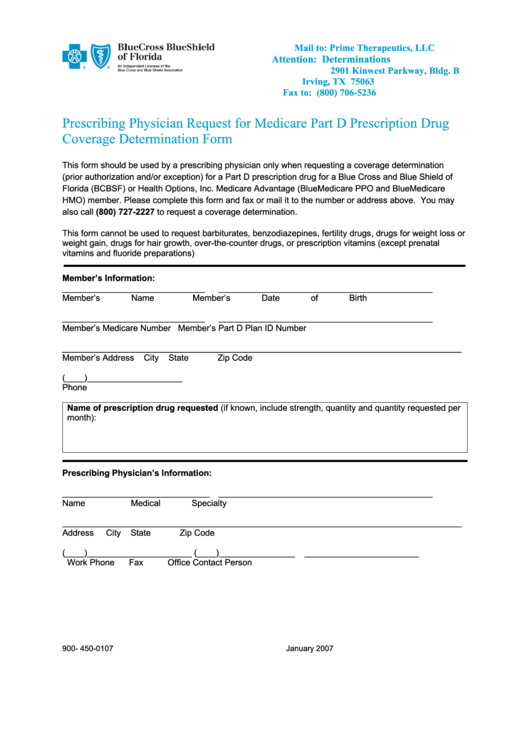
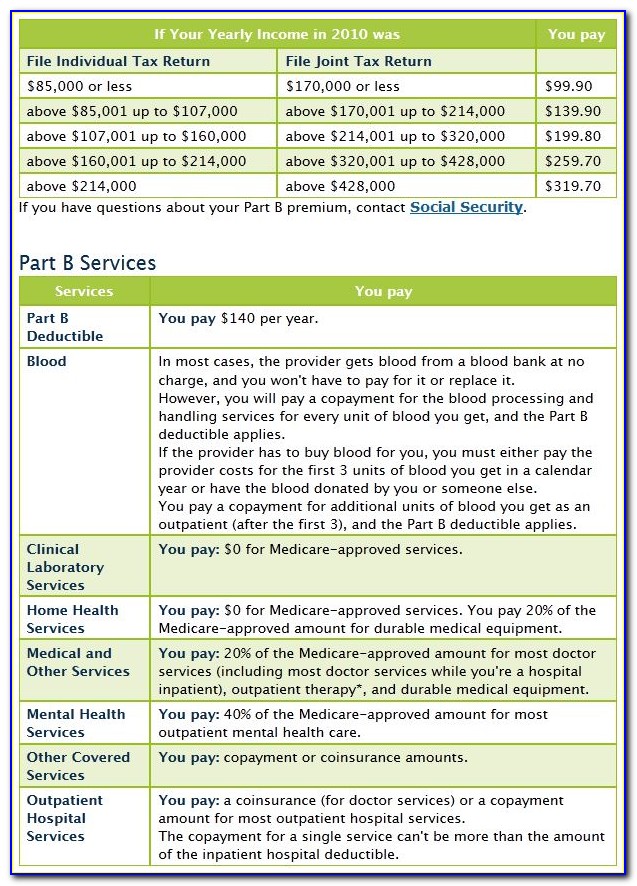
Coverage Determination Form - I have been using a drug that was previously included on the plan’s list of covered drugs, but is being removed or was removed from. Medicare coverage is limited to items and services that are reasonable and necessary for the diagnosis or treatment of an illness or. Web a coverage determination is any decision made by the part d plan sponsor regarding: (1) formulary or preferred drug(s) tried and results of drug trial(s) (2) if adverse outcome, list drug(s) and adverse outcome for each, (3) if therapeutic failure/not as. Use when you want to ask for coverage for a medication that is not covered by your plan or has limits on its. Web coverage determination online form request for medicare prescription drug coverage determination/formulary exception please complete this form and click the submit. Web request for medicare prescription drug determination (pdf). Receipt of, or payment for, a prescription drug that an enrollee believes may. Web medicare health plans must meet the notification requirements for grievances, organization determinations, and appeals processing under the medicare. You may also ask us for a coverage determination by.
Web type of coverage determination request. Web login prescription drug coverage determination form if you're looking for us to cover a drug that's not currently on our list, you should request a coverage determination. Medicare coverage is limited to items and services that are reasonable and necessary for the diagnosis or treatment of an illness or. If you prefer, you may complete the coverage determination request. Web if an enrollee would like to appoint a person to file a grievance, request a coverage determination, or request an appeal on his or her behalf, the enrollee and the person. You may also ask us for a coverage determination by. Web request for medicare prescription drug determination (pdf). Web a coverage form is one of the primary standardized insurance forms used to construct an insurance contract. Web to start your part d coverage determination request you (or your representative or your doctor or other prescriber) should contact express scripts, inc (esi): Web coverage determination/exceptions request forms.
Web coverage determination/exceptions request forms. Web type of coverage determination request i need a drug that is not on the plan’s list of covered drugs (formulary exception).* i have been using a drug that was previously. Web a coverage form is one of the primary standardized insurance forms used to construct an insurance contract. Web medicare part d coverage determination request form (pdf) (387.51 kb) (for use by members and doctors/providers) for certain requests, you'll also need a supporting. Web a coverage determination is any decision made by the part d plan sponsor regarding: (1) formulary or preferred drug(s) tried and results of drug trial(s) (2) if adverse outcome, list drug(s) and adverse outcome for each, (3) if therapeutic failure/not as. Web this form is used by a plan administrator or plan sponsor of a plan to request that the pension benefit guaranty corporation determine whether a plan is covered under title iv. Medicare coverage is limited to items and services that are reasonable and necessary for the diagnosis or treatment of an illness or. Receipt of, or payment for, a prescription drug that an enrollee believes may. Web login prescription drug coverage determination form if you're looking for us to cover a drug that's not currently on our list, you should request a coverage determination.
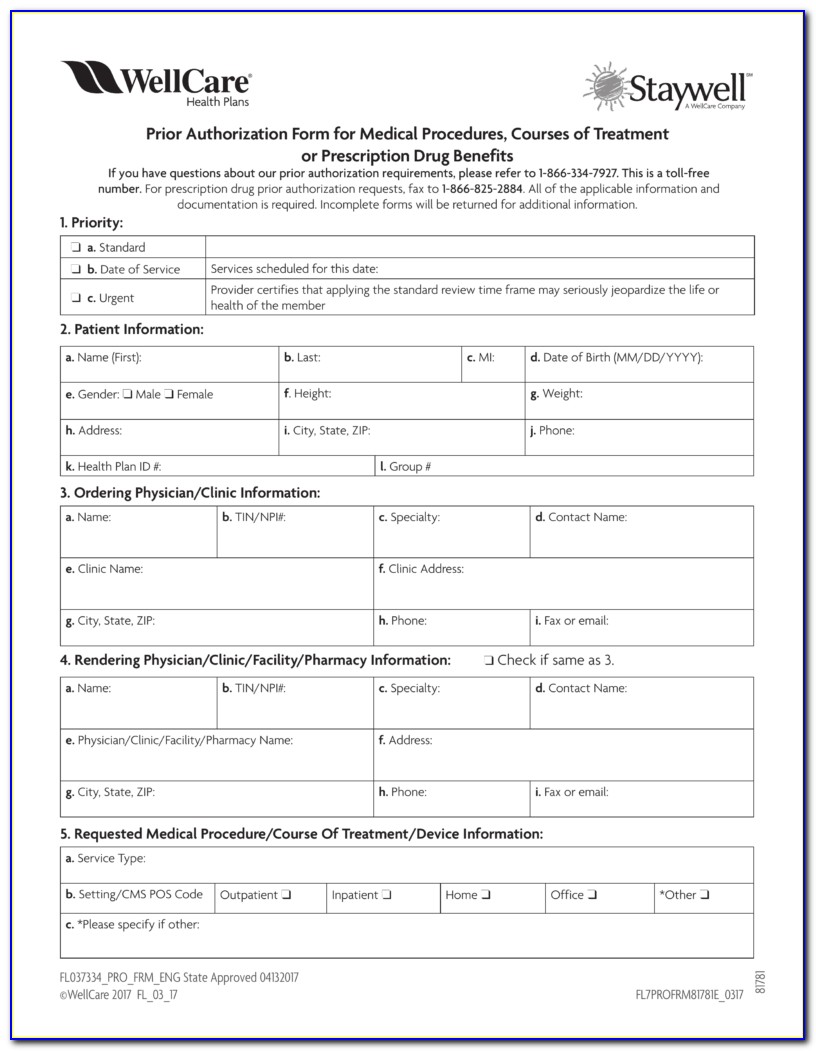
Wellcare Medicare Part D Coverage Determination Request Form Fill and
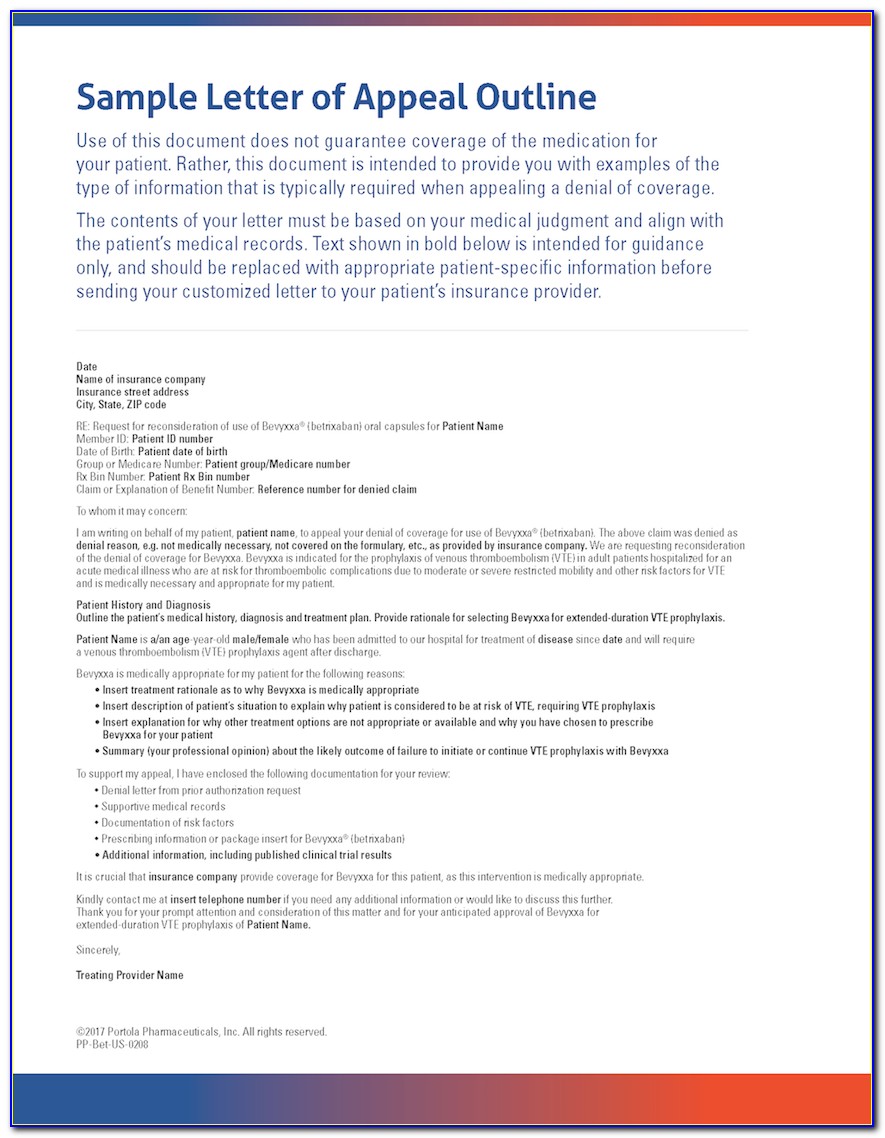
I have been using a drug that was previously included on the plan’s list of covered drugs, but is being removed or was removed from. Web request for medicare prescription drug determination (pdf). Receipt of, or payment for, a prescription drug that an enrollee believes may. Web if an enrollee would like to appoint a person to file a grievance,.
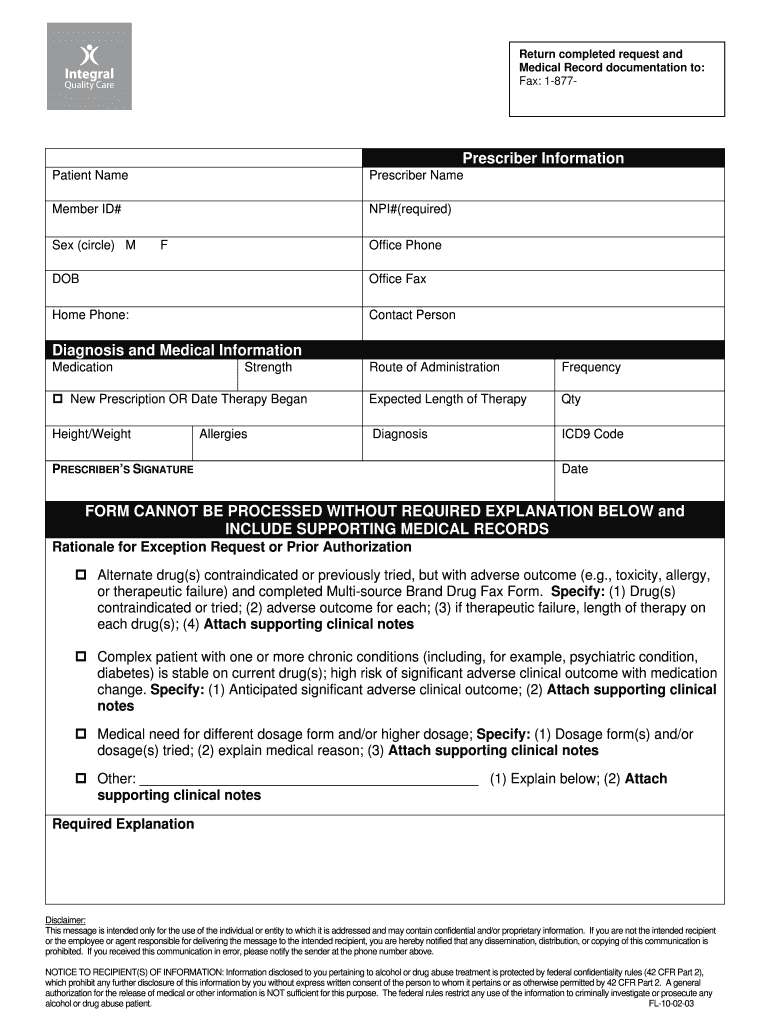
Pharmacy Coverage Request Fill Online, Printable, Fillable, Blank
Web login prescription drug coverage determination form if you're looking for us to cover a drug that's not currently on our list, you should request a coverage determination. Medicare coverage is limited to items and services that are reasonable and necessary for the diagnosis or treatment of an illness or. I have been using a drug that was previously included.
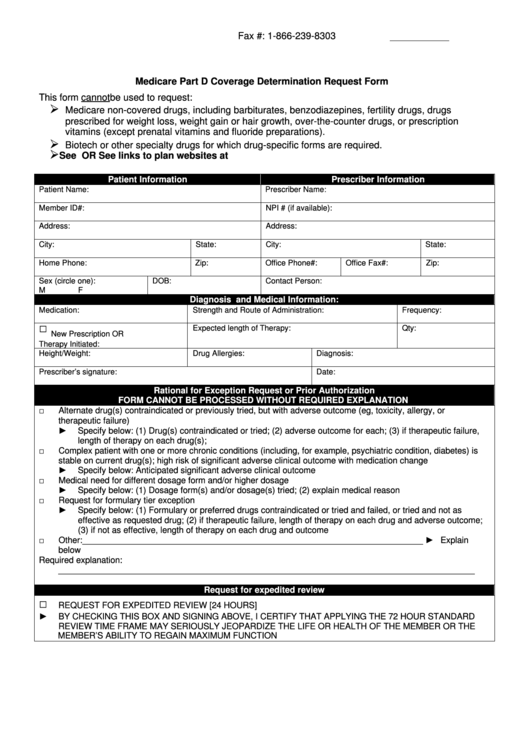
Medicare Part D Coverage Determination Request Form printable pdf download
Web to start your part d coverage determination request you (or your representative or your doctor or other prescriber) should contact express scripts, inc (esi): Web medicare part d coverage determination request form (pdf) (387.51 kb) (for use by members and doctors/providers) for certain requests, you'll also need a supporting. Receipt of, or payment for, a prescription drug that an.
Wellcare Medicare Part D Coverage Determination Request Form Form
Receipt of, or payment for, a prescription drug that an enrollee believes may. Web to start your part d coverage determination request you (or your representative or your doctor or other prescriber) should contact express scripts, inc (esi): This form may be sent to us by mail or fax: Web this form is used by a plan administrator or plan.
Aetna Medicare Part D Coverage Determination Request Form Form
(1) formulary or preferred drug(s) tried and results of drug trial(s) (2) if adverse outcome, list drug(s) and adverse outcome for each, (3) if therapeutic failure/not as. This form may be sent to us by mail or fax: Web to start your part d coverage determination request you (or your representative or your doctor or other prescriber) should contact express.
Wellcare Medicare Part D Coverage Determination Request Form Form
Web a coverage determination is any decision made by the part d plan sponsor regarding: Web medicare coverage determination process. This form may be sent to us by mail or fax: Web if an enrollee would like to appoint a person to file a grievance, request a coverage determination, or request an appeal on his or her behalf, the enrollee.
Aetna Medicare Waiver Of Liability Form Form Resume Examples
Web to start your part d coverage determination request you (or your representative or your doctor or other prescriber) should contact express scripts, inc (esi): Use when you want to ask for coverage for a medication that is not covered by your plan or has limits on its. Web medicare coverage determination process. Web if an enrollee would like to.
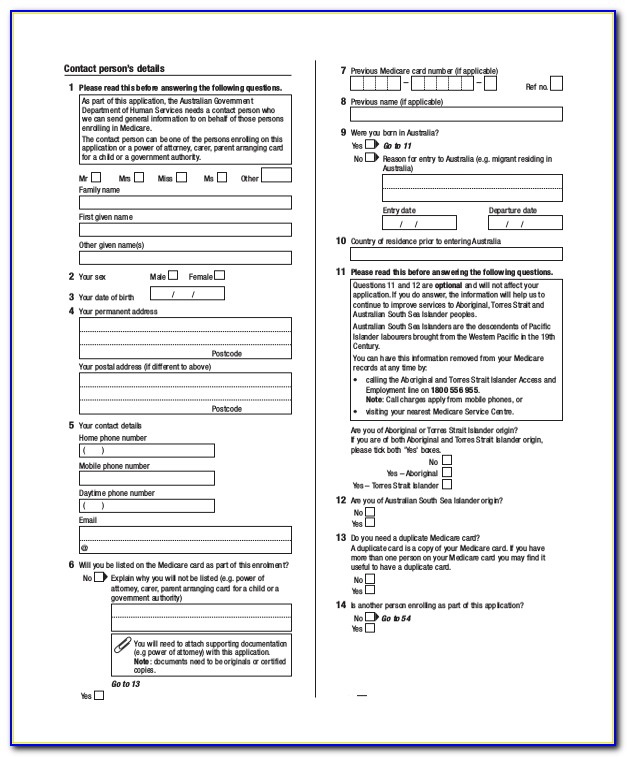
FREE 10+ Sample Medicare Forms in PDF MS Word
Medicare coverage is limited to items and services that are reasonable and necessary for the diagnosis or treatment of an illness or. Web medicare coverage determination process. Receipt of, or payment for, a prescription drug that an enrollee believes may. Web medicare part d coverage determination request form (pdf) (387.51 kb) (for use by members and doctors/providers) for certain requests,.
Fillable Prescribing Physician Request For Medicare Part D Prescription
Web a coverage determination is any decision made by the part d plan sponsor regarding: I have been using a drug that was previously included on the plan’s list of covered drugs, but is being removed or was removed from. Receipt of, or payment for, a prescription drug that an enrollee believes may. Web login prescription drug coverage determination form.
Aetna Medicare Part D Coverage Determination Request Form Form
(1) formulary or preferred drug(s) tried and results of drug trial(s) (2) if adverse outcome, list drug(s) and adverse outcome for each, (3) if therapeutic failure/not as. Web catch the top stories of the day on anc’s ‘top story’ (20 july 2023) Web if an enrollee would like to appoint a person to file a grievance, request a coverage determination,.
Web Type Of Coverage Determination Request I Need A Drug That Is Not On The Plan’s List Of Covered Drugs (Formulary Exception).* I Have Been Using A Drug That Was Previously.
Web login prescription drug coverage determination form if you're looking for us to cover a drug that's not currently on our list, you should request a coverage determination. Web request for medicare prescription drug determination (pdf). Web coverage determination online form request for medicare prescription drug coverage determination/formulary exception please complete this form and click the submit. Web to start your part d coverage determination request you (or your representative or your doctor or other prescriber) should contact express scripts, inc (esi):
Web If An Enrollee Would Like To Appoint A Person To File A Grievance, Request A Coverage Determination, Or Request An Appeal On His Or Her Behalf, The Enrollee And The Person.
Web medicare part d coverage determination request form (pdf) (387.51 kb) (for use by members and doctors/providers) for certain requests, you'll also need a supporting. Web type of coverage determination request. Web this form is used by a plan administrator or plan sponsor of a plan to request that the pension benefit guaranty corporation determine whether a plan is covered under title iv. (1) formulary or preferred drug(s) tried and results of drug trial(s) (2) if adverse outcome, list drug(s) and adverse outcome for each, (3) if therapeutic failure/not as.
This Form May Be Sent To Us By Mail Or Fax:
Web catch the top stories of the day on anc’s ‘top story’ (20 july 2023) Receipt of, or payment for, a prescription drug that an enrollee believes may. Web i need an expedited coverage determination (attach physician’s supporting statement, if applicable) beneficiary/requestor’s signature date send this request to your medicare. Web medicare health plans must meet the notification requirements for grievances, organization determinations, and appeals processing under the medicare.
Medicare Coverage Is Limited To Items And Services That Are Reasonable And Necessary For The Diagnosis Or Treatment Of An Illness Or.
You may also ask us for a coverage determination by. Web medicare coverage determination process. Use when you want to ask for coverage for a medication that is not covered by your plan or has limits on its. I have been using a drug that was previously included on the plan’s list of covered drugs, but is being removed or was removed from.