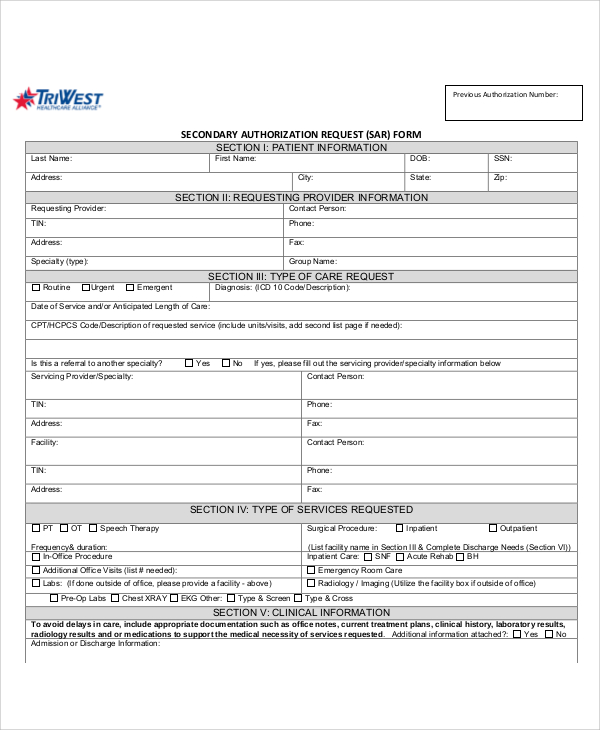
Triwest Prior Authorization Form 2022
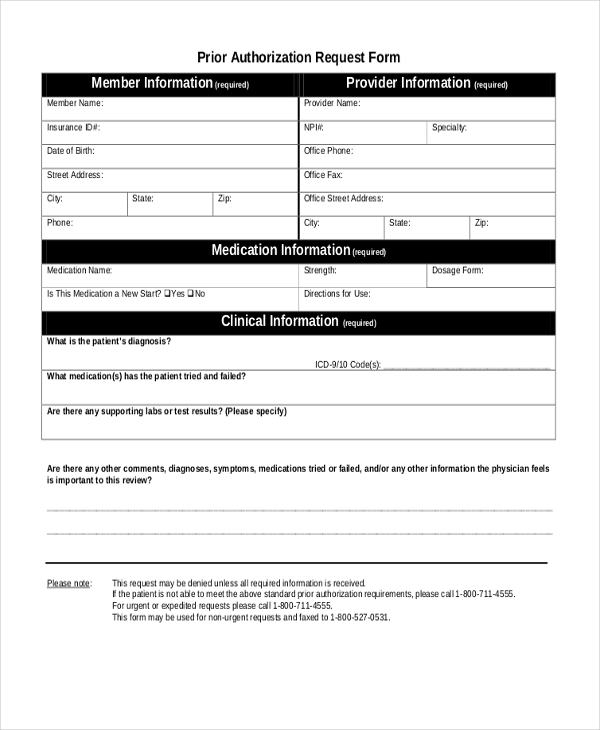
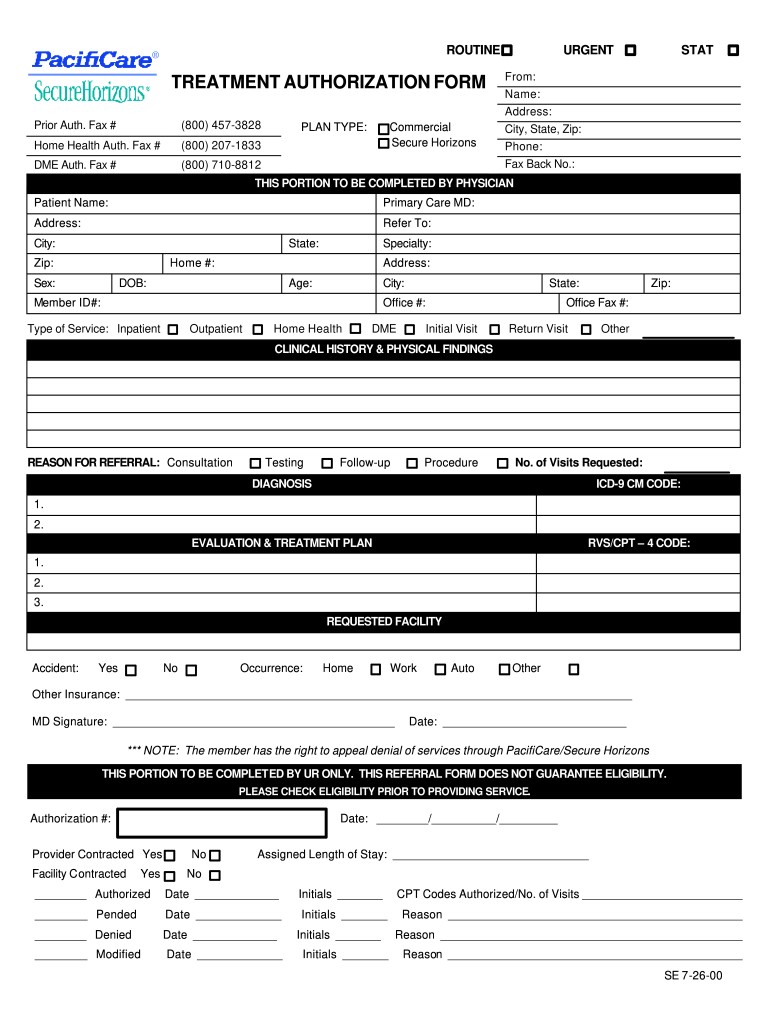
Triwest Prior Authorization Form 2022 - Your vamc may require an rfs. Type text, add images, blackout confidential details, add comments, highlights and more. Web welcome from triwest healthcare alliance. Triwest is on a mission to serve ® our nation’s veterans and military community in partnership with the department of veterans. Web how to fill out and sign va triwest authorization form online? Get your online template and fill it in using progressive features. Triwest will continue to pay pc3 claims on approved referrals for dates of service. Web use our prior authorization, referral and benefit tool. Edit your triwest forms online type text, add images, blackout confidential details, add comments, highlights and more. Verify approval requirements request changes to my authorization file an appeal complete letters of attestation review line of duty (lod) care transfer and.
Web how to fill out and sign va triwest authorization form online? Release of information (authorization to. Web use our prior authorization, referral and benefit tool. Triwest contacts the ccn provider on behalf of the. Take advantage of the tools we offer to fill out your document. Web we know pa requests are complex. Web triwest appointing veteran’s vamc approves care and delegates the appointment process to triwest. Our ancillary services approval requirements tool tells. Triwest will continue to pay pc3 claims on approved referrals for dates of service. That's why we have a team of experts and a variety of help resources to make requests faster and easier.
Verify approval requirements request changes to my authorization file an appeal complete letters of attestation review line of duty (lod) care transfer and. Pacific territories on march 31, 2022. Triwest will continue to pay pc3 claims on approved referrals for dates of service. Edit your triwest forms online type text, add images, blackout confidential details, add comments, highlights and more. Is it an ancillary service, such as diagnostic radiology or lab tests? Web use our prior authorization, referral and benefit tool. The veteran must have an approved referral/authorization from the department of veterans affairs (va) before an appointment can be set and an authorization letter. Web dental providers with practices in region 4 and 5 interested in serving veterans in their community should contact triwest. We use it to make sure your prescription drug is: Web triwest appointing veteran’s vamc approves care and delegates the appointment process to triwest.
97 LETTER OF AUTHORIZATION VALIDITY, LETTER AUTHORIZATION OF VALIDITY
Sign it in a few clicks draw your signature, type it,. Web veterans affairs community care program forms. Type text, add images, blackout confidential details, add comments, highlights and more. Web if the veteran needs a medication that’s not on va’s national formulary, the provider needs to contact the veteran’s authorizing vamc, request a formulary request review form,. Your vamc.
Bcbs Prior Auth Forms Florida Form Resume Examples A4kn4J95jG
Enjoy smart fillable fields and interactivity. Web use our prior authorization, referral and benefit tool. Web veterans affairs community care program forms. Web if the veteran needs a medication that’s not on va’s national formulary, the provider needs to contact the veteran’s authorizing vamc, request a formulary request review form,. Sign it in a few clicks draw your signature, type.
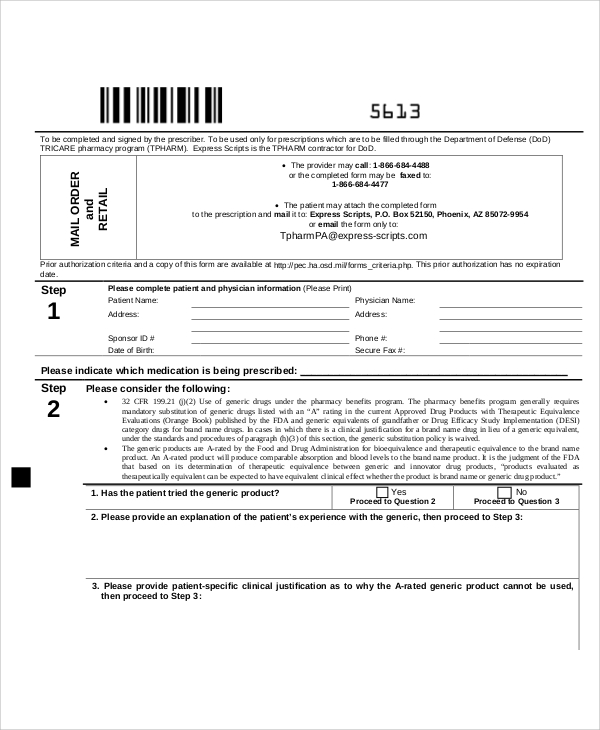
FREE 10+ Sample Medicare Forms in PDF MS Word
Web welcome from triwest healthcare alliance. The veteran must have an approved referral/authorization from the department of veterans affairs (va) before an appointment can be set and an authorization letter. Our ancillary services approval requirements tool tells. Verify approval requirements request changes to my authorization file an appeal complete letters of attestation review line of duty (lod) care transfer and..
Bcbs Prior Authorization Form Tennessee Form Resume Examples
We use it to make sure your prescription drug is: Web dental providers with practices in region 4 and 5 interested in serving veterans in their community should contact triwest. Web welcome from triwest healthcare alliance. Edit your secondary authorization request form online. Web locate triwest prior authorization and click on get form to get started.
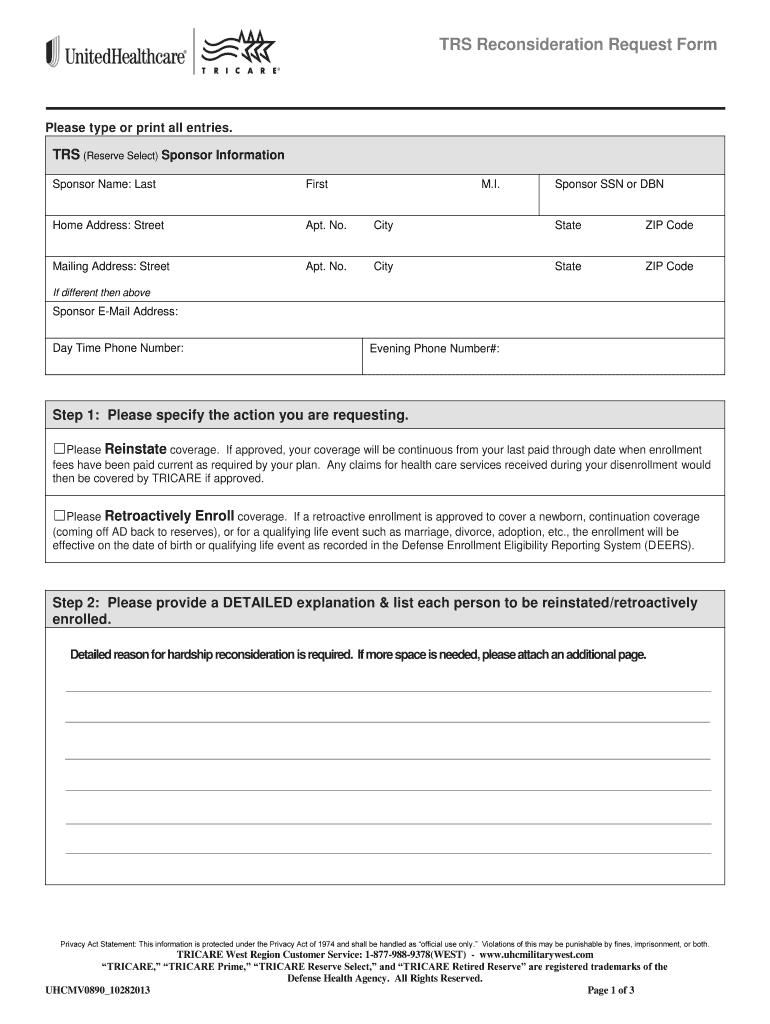
United Healthcare Prior Authorization Form Pdf Fill Out and Sign
Sign it in a few clicks. The veteran must have an approved referral/authorization from the department of veterans affairs (va) before an appointment can be set and an authorization letter. That's why we have a team of experts and a variety of help resources to make requests faster and easier. Web dental providers with practices in region 4 and 5.
Medicare Generation Rx Prior Authorization Form Form Resume
Your vamc may require an rfs. Take advantage of the tools we offer to fill out your document. Web we know pa requests are complex. Triwest contacts the ccn provider on behalf of the. Web triwest appointing veteran’s vamc approves care and delegates the appointment process to triwest.
FREE 10+ Sample Authorization Request Forms in MS Word PDF
That's why we have a team of experts and a variety of help resources to make requests faster and easier. Edit your secondary authorization request form online. Edit your triwest forms online type text, add images, blackout confidential details, add comments, highlights and more. Triwest will continue to pay pc3 claims on approved referrals for dates of service. Web how.
TriWest PC3 Secondary Authorization Request Fill and Sign Printable
Sign it in a few clicks. Web if the veteran needs a medication that’s not on va’s national formulary, the provider needs to contact the veteran’s authorizing vamc, request a formulary request review form,. Triwest is on a mission to serve ® our nation’s veterans and military community in partnership with the department of veterans. Type text, add images, blackout.
Triwest Reconsideration Form Fill Online, Printable, Fillable, Blank
Release of information (authorization to. Web how to fill out and sign va triwest authorization form online? Sign it in a few clicks. Sign it in a few clicks draw your signature, type it,. Triwest will continue to pay pc3 claims on approved referrals for dates of service.
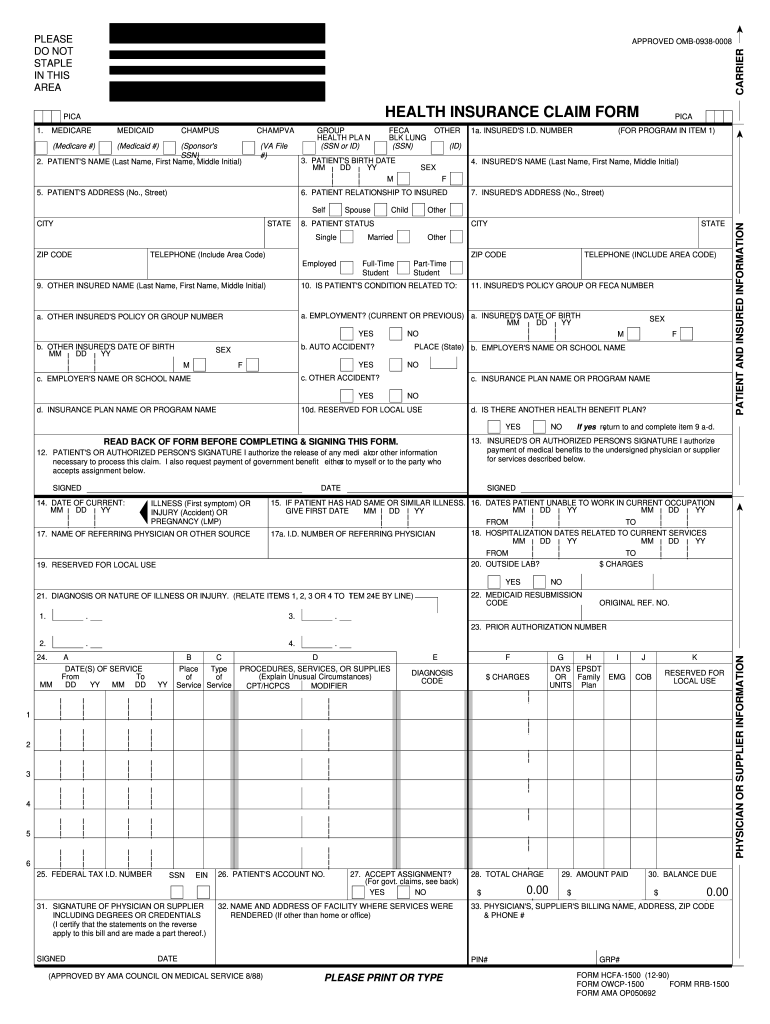
Hcfa Form Fill Out and Sign Printable PDF Template signNow
Web how to fill out and sign va triwest authorization form online? The veteran must have an approved referral/authorization from the department of veterans affairs (va) before an appointment can be set and an authorization letter. Our ancillary services approval requirements tool tells. Verify approval requirements request changes to my authorization file an appeal complete letters of attestation review line.
The Veteran Must Have An Approved Referral/Authorization From The Department Of Veterans Affairs (Va) Before An Appointment Can Be Set And An Authorization Letter.
Get your online template and fill it in using progressive features. Triwest contacts the ccn provider on behalf of the. Sign it in a few clicks. Your vamc may require an rfs.
Type Text, Add Images, Blackout Confidential Details, Add Comments, Highlights And More.
Web pc3 officially ended in alaska and the u.s. Web if the veteran needs a medication that’s not on va’s national formulary, the provider needs to contact the veteran’s authorizing vamc, request a formulary request review form,. Web triwest appointing veteran’s vamc approves care and delegates the appointment process to triwest. We use it to make sure your prescription drug is:
Web How To Fill Out And Sign Va Triwest Authorization Form Online?
Release of information (authorization to. Web we know pa requests are complex. Highlight relevant paragraphs of your. Web welcome from triwest healthcare alliance.
Triwest Will Continue To Pay Pc3 Claims On Approved Referrals For Dates Of Service.
That's why we have a team of experts and a variety of help resources to make requests faster and easier. Our ancillary services approval requirements tool tells. Take advantage of the tools we offer to fill out your document. Pacific territories on march 31, 2022.