Health Alliance Appeal Form
Health Alliance Appeal Form - Web this form can be used to ask alliance to reconsider a decision to deny a service request. Web the provider request for reconsideration form is posted on the alliance web site and serves as a cover page to the provider appeal. If you have any questions, or if you’re unable to find what you’re looking for, contact us. Web for dates of service august 1, 2021 and after, the appeals process will now have one level of formal appeal after first asking for an informal inquiry on a denied. Web here you’ll find forms relating to your medicare plan. Uha and our providers will not stop you from filing a complaint, appeal or hearing. Incomplete or illegible information will. The questions and answers below will provide additional information and instruction. Web the hearing was particularly timely, because the u.s. Please include any supporting documents, notes, statements, and medical.
The questions and answers below will provide additional information and instruction. Web request form medical records must accompany all requests to be completed for all requests. Alliance will acknowledge receipt of. Umpqua health alliance (uha) cares about you and your health. Web for information on submitting claims, visit our updated where to submit claims webpage. Web to submit a formal appeal, you must complete the provider appeal form located at provider.healthalliance.org. If we deny your request for a coverage decision or payment, you have the right to request an appeal. Web a written request for a reconsideration of the decision must be submitted to health alliance within 60 days from the date of denial notice from health alliance. If you have any questions, or if you’re unable to find what you’re looking for, contact us. Web appeals, grievances, & hearings.
Web online claims reprocessing inquiry, as mentioned above, you may submit a formal appeal to us within 90 days from the original denial, unless otherwise stated in your contract. If we deny your request for a coverage decision or payment, you have the right to request an appeal. Web appeals, grievances, & hearings. Web for information on submitting claims, visit our updated where to submit claims webpage. Web to file or check the status of a grievance or an appeal‚ contact us at: Web this handout was developed in part under a grant from the health resources and services administration (hrsa), u.s. Cotiviti and change healthcare/tc3 claims denial appeal form; Web our process for accepting and responding to appeals. Web member appeal form complete this form if you are appealing the outcome of a processed medical need. Web to submit a formal appeal, you must complete the provider appeal form located at provider.healthalliance.org.
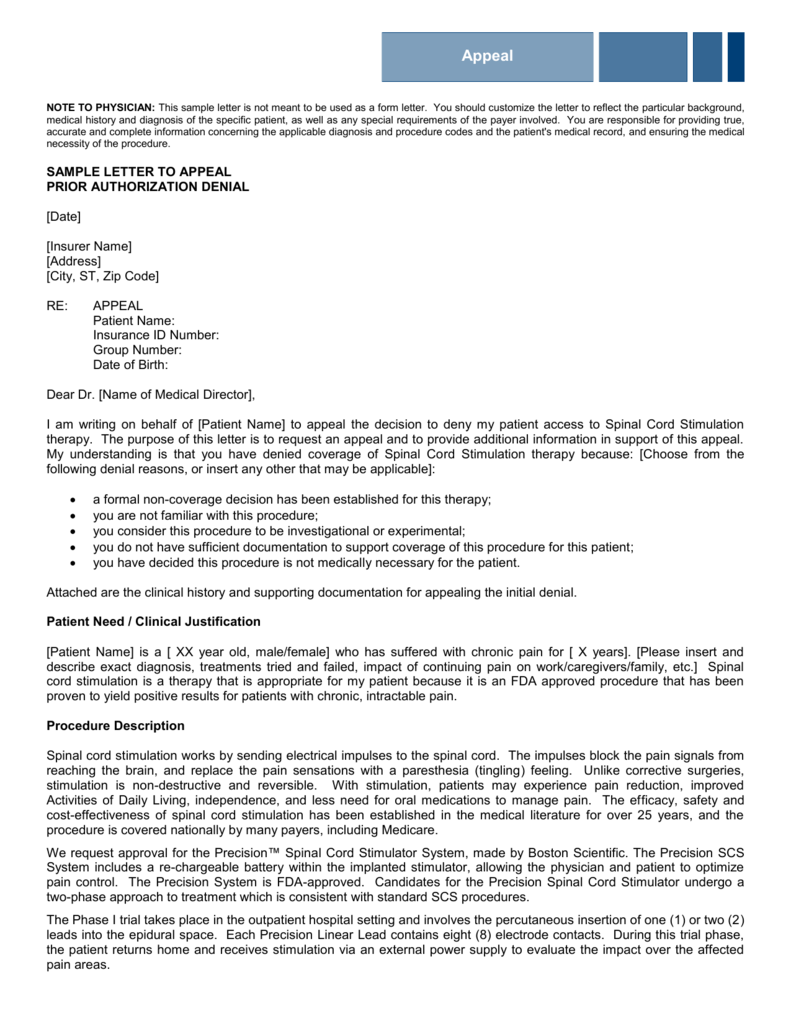
Sample Appeal Letter For Medical Claim Denial designerwrapper
Web our process for accepting and responding to appeals. Alliance will acknowledge receipt of. Web this form can be used to ask alliance to reconsider a decision to deny a service request. Web health alliance credentialing application (for contracted midlevel providers) caqh provider addition form (for il contracted mds and dos only) ancillary facility checklist. In your local time zone.
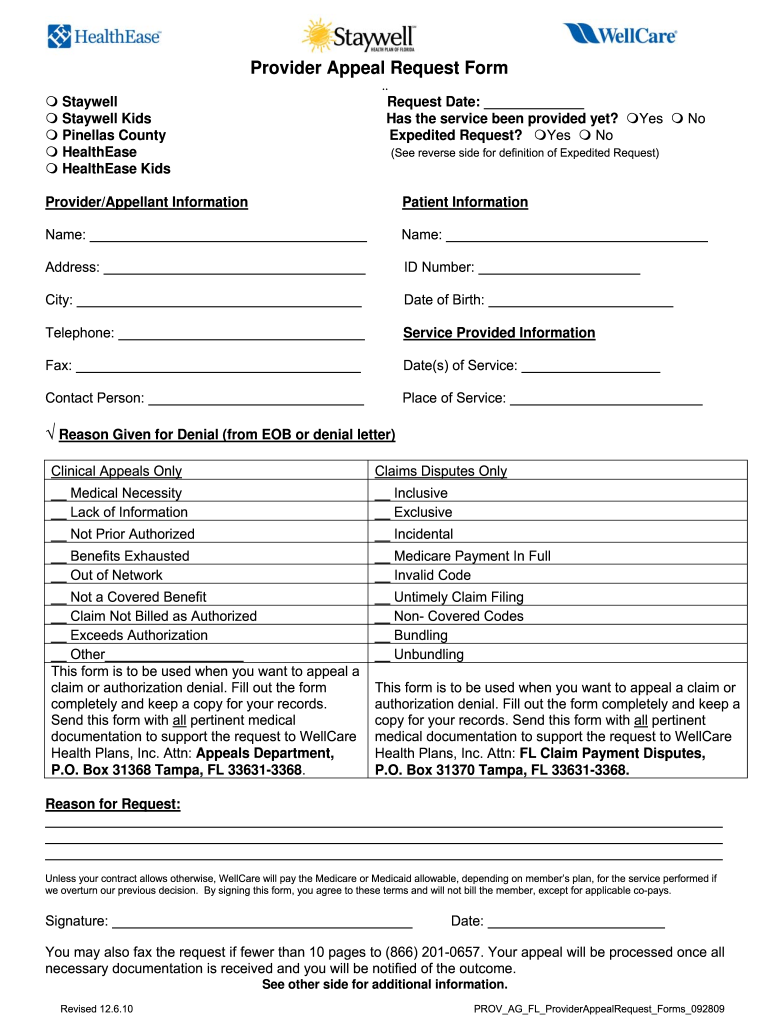
Wellcare Appeal Form Fill Online, Printable, Fillable, Blank pdfFiller
Please include any supporting documents, notes, statements, and medical. Incomplete or illegible information will. Web community care network contact centerproviders and va staff only. Complete the form below with your alliance information. The questions and answers below will provide additional information and instruction.
Health Alliance Appeal Form Doctor Heck
Web member appeal form complete this form if you are appealing the outcome of a processed medical need. Once the appeal form has been completed,. Incomplete or illegible information will. Web the provider request for reconsideration form is posted on the alliance web site and serves as a cover page to the provider appeal. Complete the form below with your.
Health Alliance Medicare Prior Authorization Form Doctor Heck
Web community care network contact centerproviders and va staff only. Web health alliance credentialing application (for contracted midlevel providers) caqh provider addition form (for il contracted mds and dos only) ancillary facility checklist. Web online claims reprocessing inquiry, as mentioned above, you may submit a formal appeal to us within 90 days from the original denial, unless otherwise stated in.
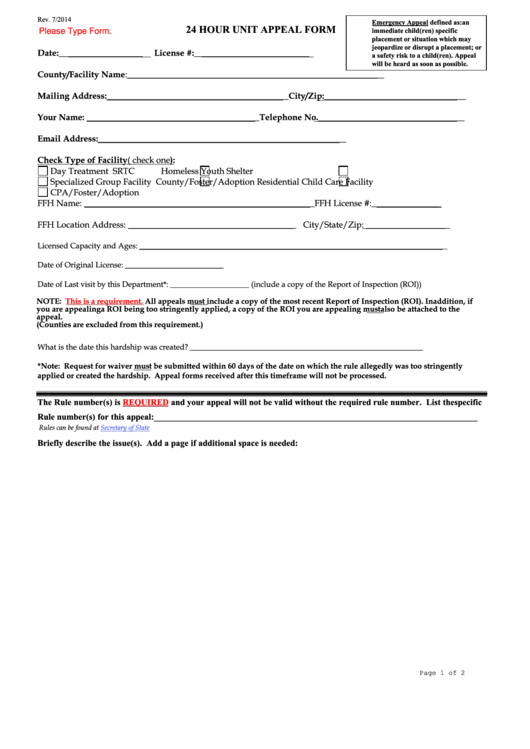
Fillable 24 Hour Unit Appeal Form Colorado Department Of Human
Umpqua health alliance (uha) cares about you and your health. Is facing intensifying urgency to stop the worsening fentanyl epidemic. Web we want it to be easy for you to work with hap. Please include any supporting documents, notes, statements, and medical. Alliance will acknowledge receipt of.
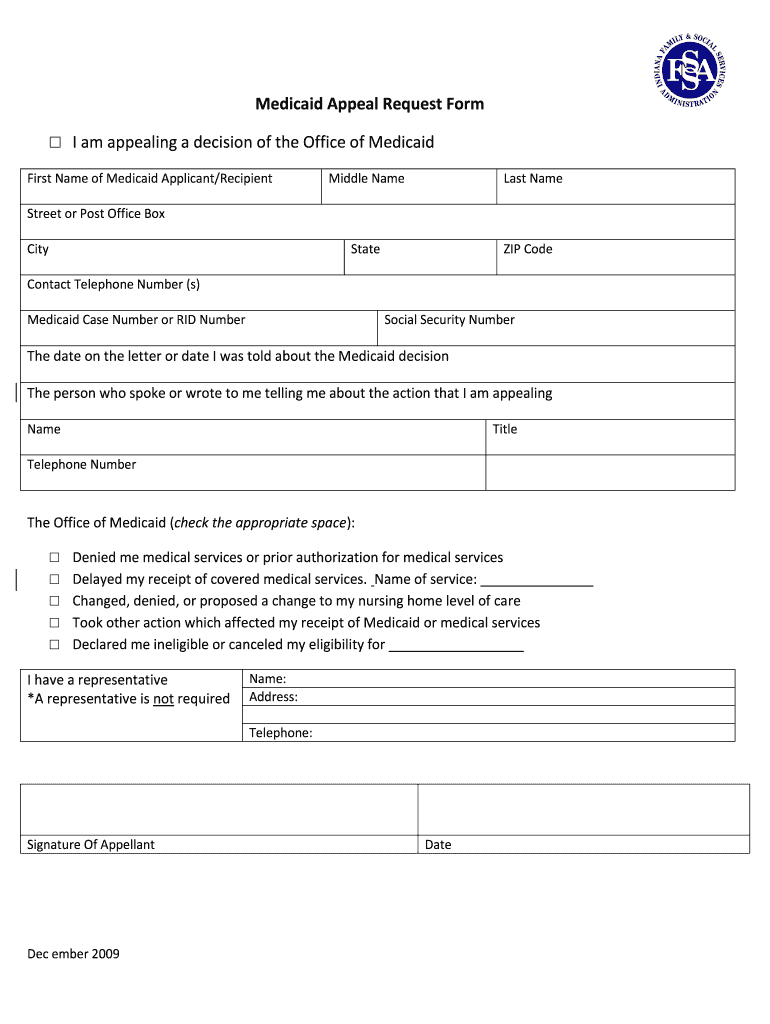
Indiana Medicaid Appeal Form Fill Online, Printable, Fillable, Blank
The questions and answers below will provide additional information and instruction. Web our process for accepting and responding to appeals. Here are forms you'll need: Web appeals, grievances, & hearings. Please include any supporting documents, notes, statements, and medical.
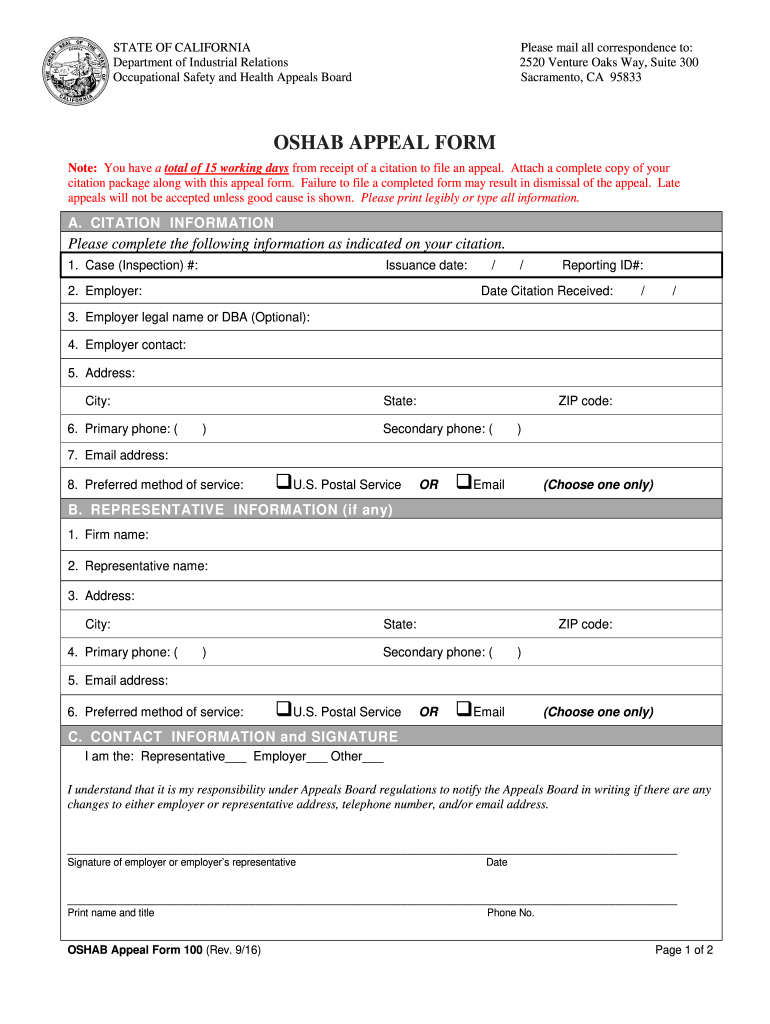
Cal Osha Appeal's Form C Om Fill Out and Sign Printable PDF Template
Web we want it to be easy for you to work with hap. Web here you’ll find forms relating to your medicare plan. Web request form medical records must accompany all requests to be completed for all requests. Drug deaths nationwide hit a record. Web to file or check the status of a grievance or an appeal‚ contact us at:
Health Insurance Marketplace Appeal Request Form 0 Printable Blank
Of health and human services (hhs) grant. Provider network management section 3: Is facing intensifying urgency to stop the worsening fentanyl epidemic. If we deny your request for a coverage decision or payment, you have the right to request an appeal. Web a written request for a reconsideration of the decision must be submitted to health alliance within 60 days.
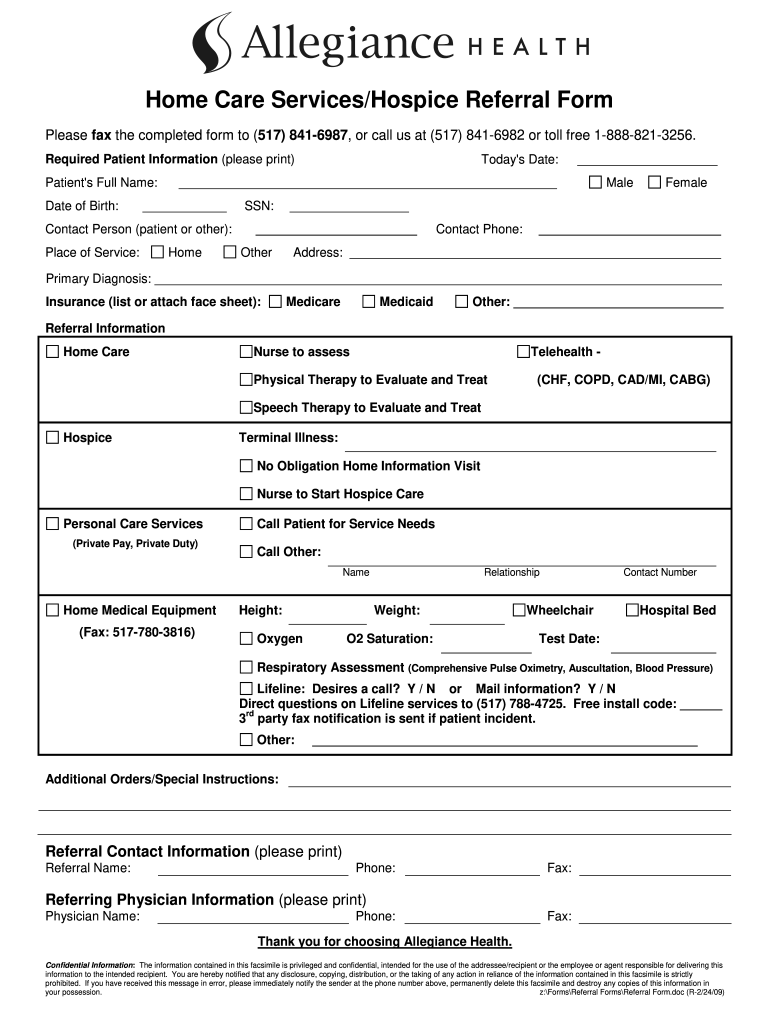
Home Health Referral Form Template Fill Out and Sign Printable PDF
Web to file or check the status of a grievance or an appeal‚ contact us at: Umpqua health alliance (uha) cares about you and your health. If you have any questions, or if you’re unable to find what you’re looking for, contact us. Complete the form below with your alliance information. Web a written request for a reconsideration of the.
Cigna Appeal Form Fill Online, Printable, Fillable, Blank pdfFiller
If you have any questions, or if you’re unable to find what you’re looking for, contact us. Web the provider request for reconsideration form is posted on the alliance web site and serves as a cover page to the provider appeal. Complete the form below with your alliance information. Incomplete or illegible information will. If we deny your request for.
Web Appeals, Grievances, & Hearings.
Please choose the type of. If we deny your request for a coverage decision or payment, you have the right to request an appeal. Web the hearing was particularly timely, because the u.s. Of health and human services (hhs) grant.
Web Here You’ll Find Forms Relating To Your Medicare Plan.
Provider network management section 3: Web community care network contact centerproviders and va staff only. Web this form can be used to ask alliance to reconsider a decision to deny a service request. Web online claims reprocessing inquiry, as mentioned above, you may submit a formal appeal to us within 90 days from the original denial, unless otherwise stated in your contract.
Web To Submit A Formal Appeal, You Must Complete The Provider Appeal Form Located At Provider.healthalliance.org.
Web health alliance credentialing application (for contracted midlevel providers) caqh provider addition form (for il contracted mds and dos only) ancillary facility checklist. Web for dates of service august 1, 2021 and after, the appeals process will now have one level of formal appeal after first asking for an informal inquiry on a denied. Complete the form below with your alliance information. Web this handout was developed in part under a grant from the health resources and services administration (hrsa), u.s.
Web To File Or Check The Status Of A Grievance Or An Appeal‚ Contact Us At:
Web a written request for a reconsideration of the decision must be submitted to health alliance within 60 days from the date of denial notice from health alliance. The questions and answers below will provide additional information and instruction. Web request form medical records must accompany all requests to be completed for all requests. Incomplete or illegible information will.