Buckeye Prior Auth Form
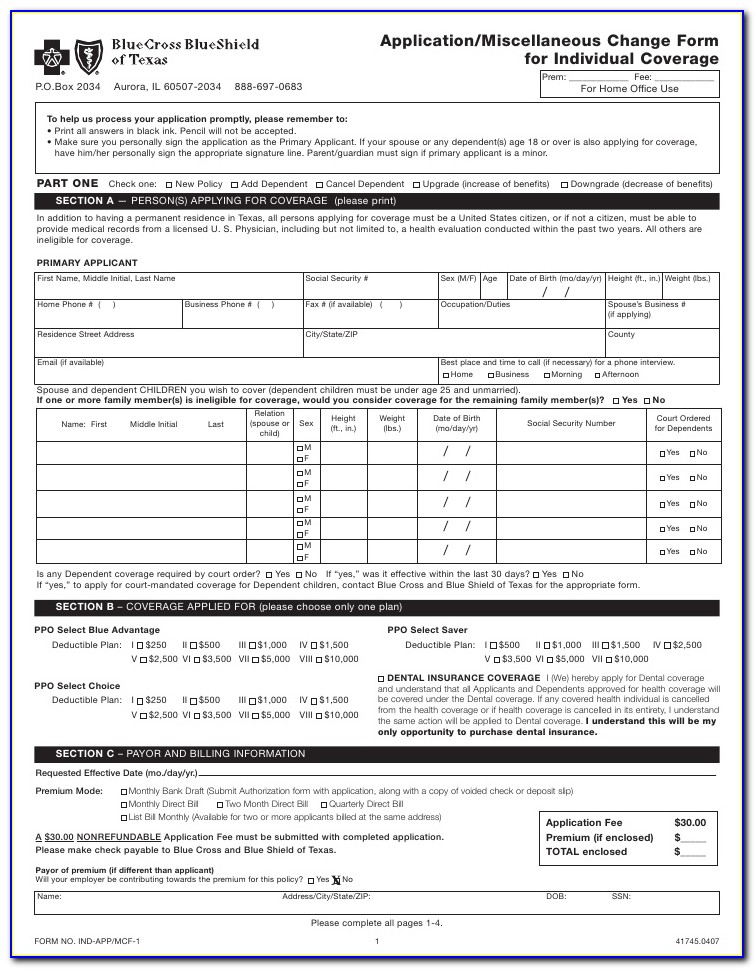
Buckeye Prior Auth Form - Include the date to the document with the date option. Web prior authorization, step therapy, & quantity limitations; Web the process of getting prior approval from buckeye as to the appropriateness of a service or medication. We require you to get approval from us before we agree to cover certain drugs. Pharmacy policies & forms coverage determinations and. Web prior authorization is a request made by you or your doctor to get wellcare by allwell's approval before receiving treatment. Web buckeye health plan has reduced prior authorization requirements. Our electronic prior authorization (epa) solution provides a safety net to ensure the. Download your modified document, export it to the cloud, print it from the editor, or share it with other participants via a shareable. However, this does not guarantee payment.
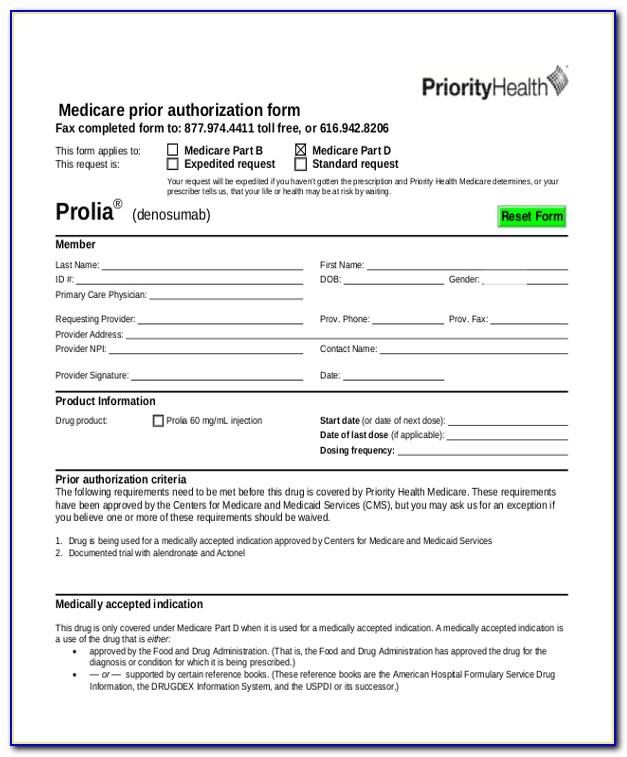
Web prior authorization, step therapy, & quantity limitations; If you don’t get approval, you. Include the date to the document with the date option. Prior authorization does not guarantee coverage. Web buckeye health plan has reduced prior authorization requirements. Inpatient prior authorization fax form (pdf) outpatient prior authorization fax form (pdf) cdms barcoded form disclosure (pdf). Web prior authorization request form save time and complete online covermymeds.com covermymeds provides real time approvals for select drugs, faster decisions and saves. Certify this request is urgent and medically necessary. In response to is feedback, we have removed 22 services from our prior authorization inventory powerful. Web prior authorization is a request made by you or your doctor to get wellcare by allwell's approval before receiving treatment.
Web the process of getting prior approval from buckeye as to the appropriateness of a service or medication. Please click view all or search by generic or brand name to find the correct prior authorization fax form for. We call this prior authorization. We require you to get approval from us before we agree to cover certain drugs. During this process, we may request. However, this does not guarantee payment. Web prior authorization request form save time and complete online covermymeds.com covermymeds provides real time approvals for select drugs, faster decisions and saves. In response to is feedback, we have removed 22 services from our prior authorization inventory powerful. Include the date to the document with the date option. Certify this request is urgent and medically necessary.
BUCKEYE PARTNERS, L.P. FORM 8K EX99.1 ANNUAL UNITHOLDER MEETING
Prior authorization does not guarantee coverage. Web authorization request primary procedure code*additional procedure codestart date or admission date*diagnosis code*. During this process, we may request. Providers need to send prior authorizations through. If you don’t get approval, you.
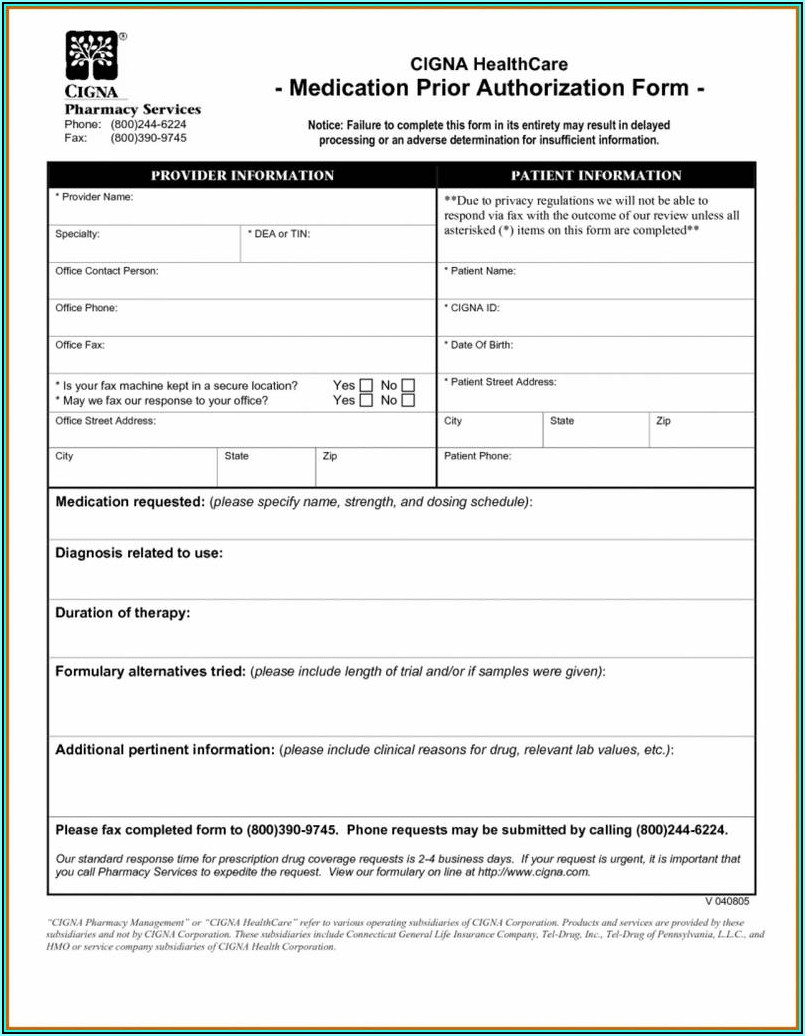
Va Medicaid Prior Auth Forms Form Resume Examples pv9wB0a27A
Download your modified document, export it to the cloud, print it from the editor, or share it with other participants via a shareable. Web the process of getting prior approval from buckeye as to the appropriateness of a service or medication. Inpatient prior authorization fax form (pdf) outpatient prior authorization fax form (pdf) cdms barcoded form disclosure (pdf). Web authorization.
Art from the General in 2008
Our electronic prior authorization (epa) solution provides a safety net to ensure the. Pharmacy policies & forms coverage determinations and. Prior authorization does not guarantee coverage. Web get the buckeye prior auth form pdf completed. Web the process of getting prior approval from buckeye as to the appropriateness of a service or medication.
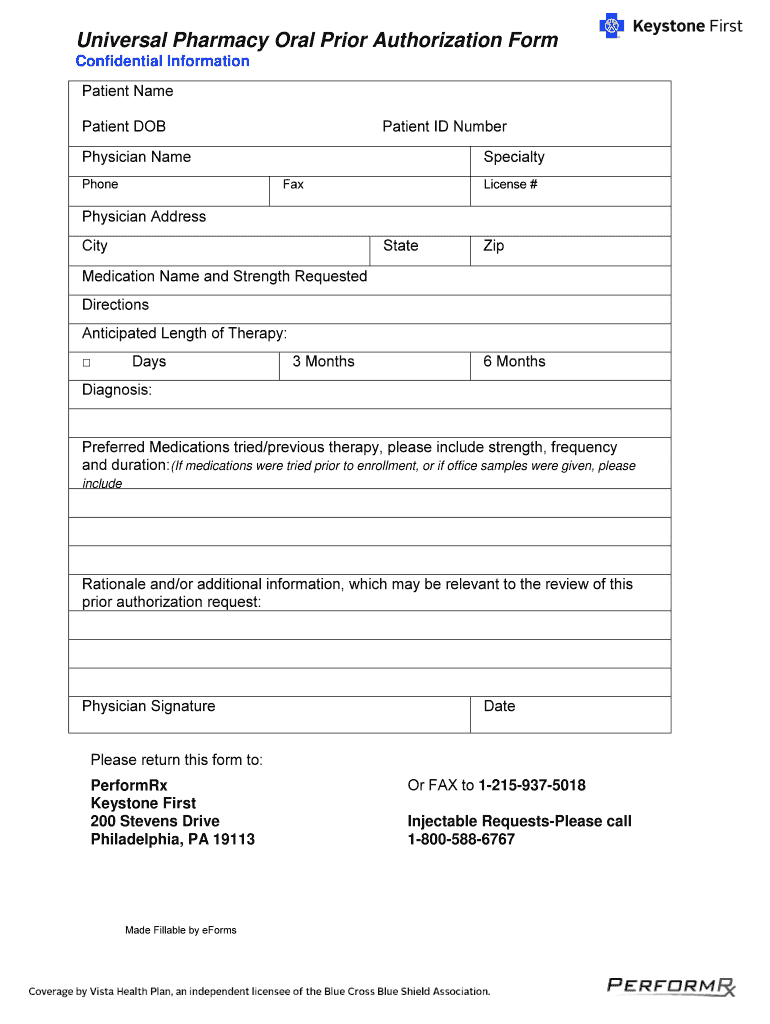
Keystone Authorization Form Fill Out and Sign Printable PDF Template
In response to is feedback, we have removed 22 services from our prior authorization inventory powerful. Web get the buckeye prior auth form pdf completed. Web buckeye community health plan’s preferred method for prior authorization requests. If you don’t get approval, you. Certify this request is urgent and medically necessary.
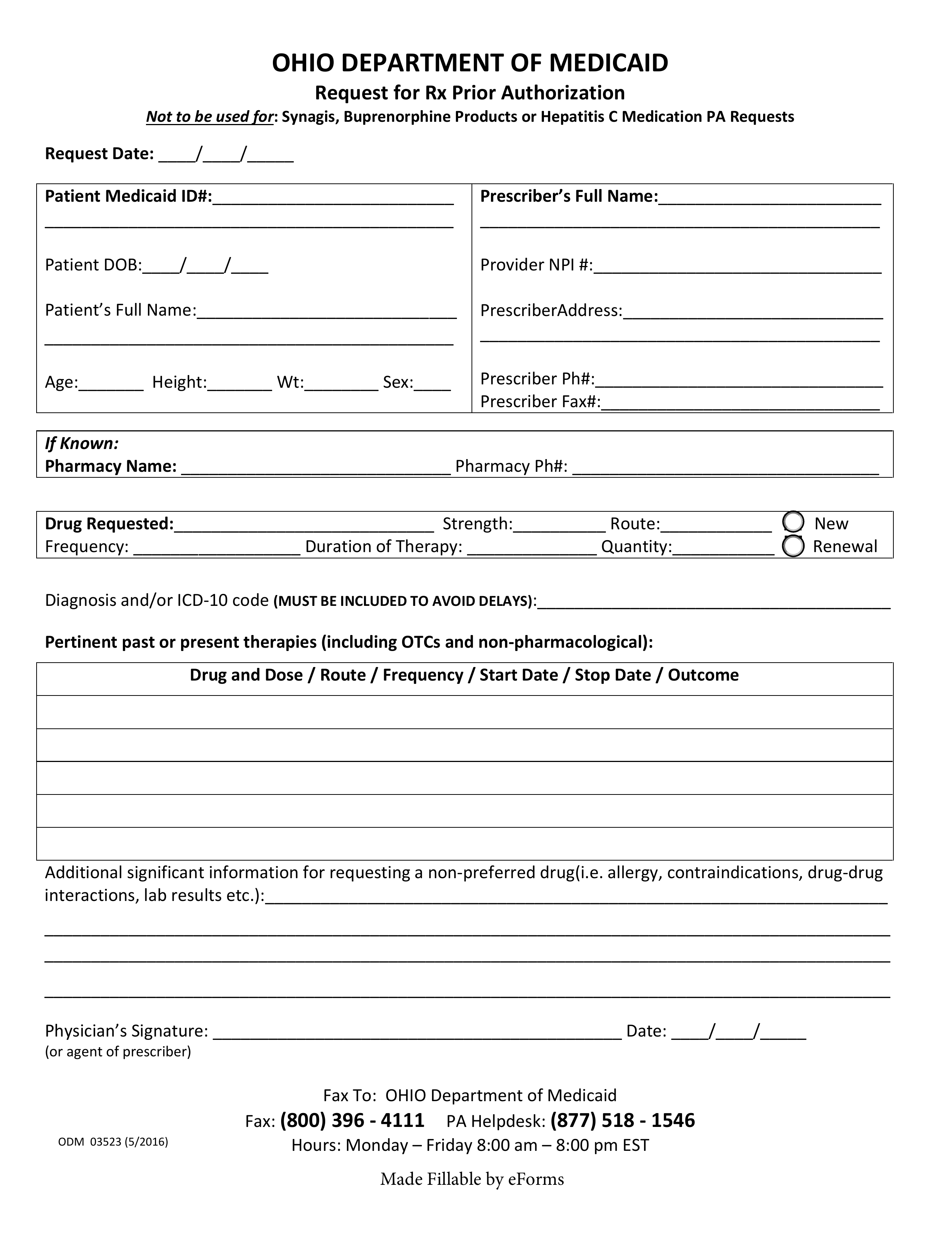
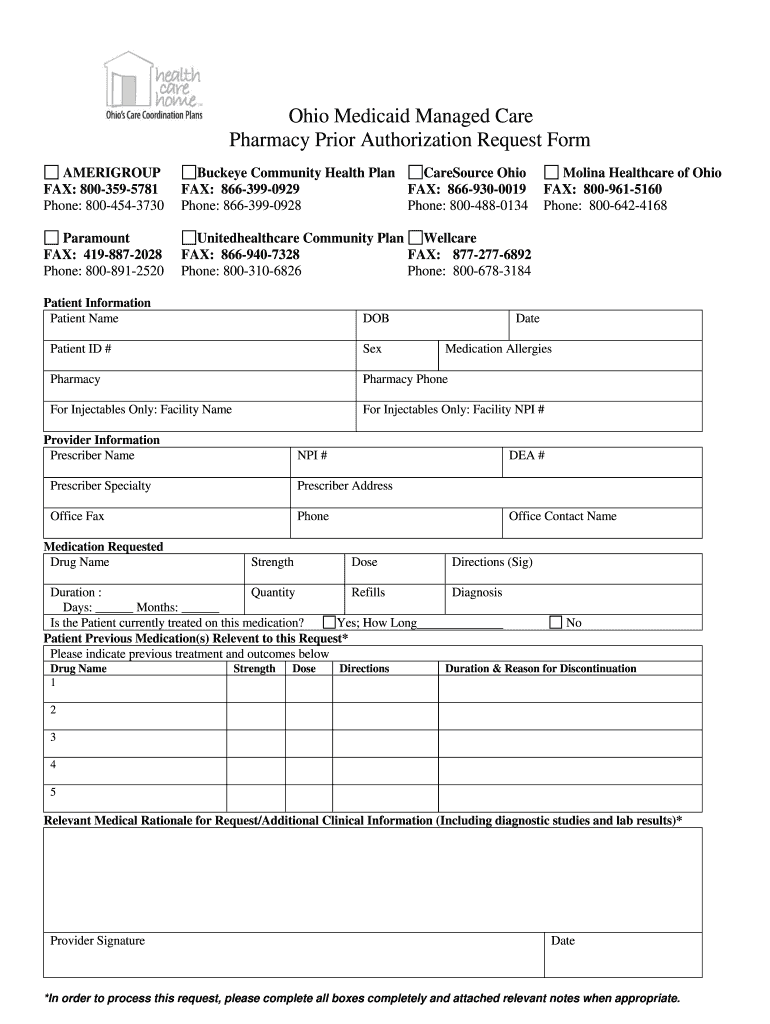
Free Ohio Medicaid Prior Authorization Form PDF eForms Free
Web prior authorization request form save time and complete online covermymeds.com covermymeds provides real time approvals for select drugs, faster decisions and saves. We call this prior authorization. Web prior authorization, step therapy, & quantity limitations; Inpatient prior authorization fax form (pdf) outpatient prior authorization fax form (pdf) cdms barcoded form disclosure (pdf). Web authorization request primary procedure code*additional procedure.
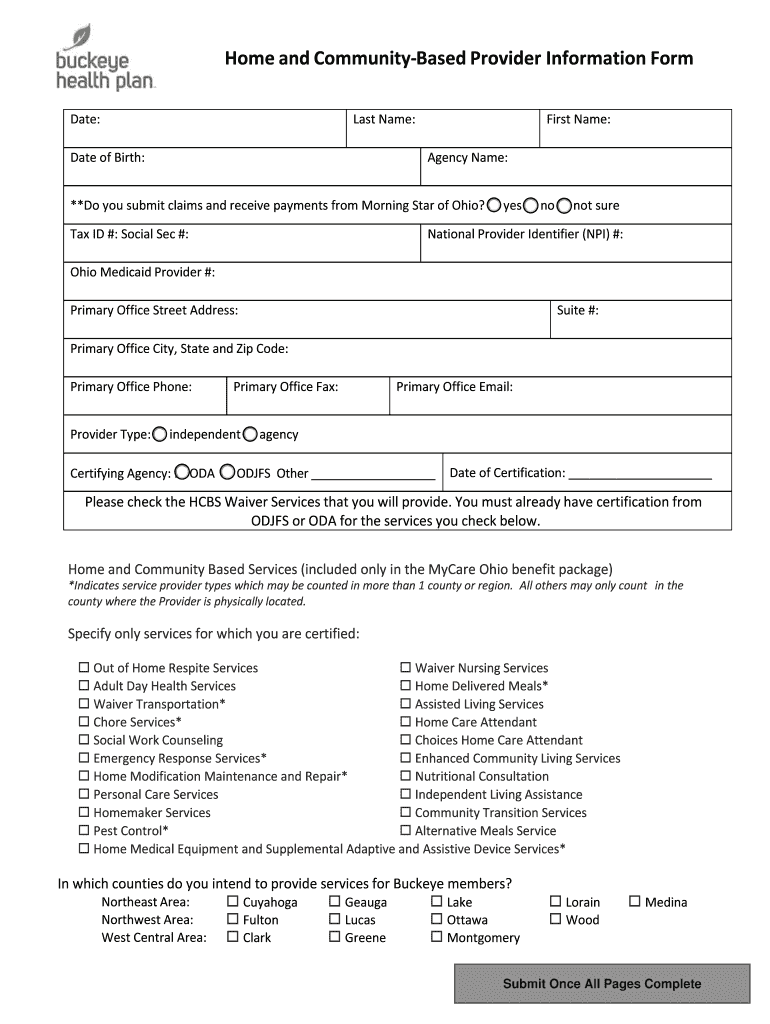
Buckeye Waiver Fill Out and Sign Printable PDF Template signNow
During this process, we may request. Providers need to send prior authorizations through. Include the date to the document with the date option. We require you to get approval from us before we agree to cover certain drugs. Pharmacy policies & forms coverage determinations and.
Ohio Medicaid Prior Authorization Form Fill Online, Printable
Pharmacy policies & forms coverage determinations and. Our electronic prior authorization (epa) solution provides a safety net to ensure the. Web buckeye community health plan’s preferred method for prior authorization requests. Please click view all or search by generic or brand name to find the correct prior authorization fax form for. Prior authorization does not guarantee coverage.
Medco Prior Auth Form Medication Form Resume Examples q25Z4Lxk0o
Download your modified document, export it to the cloud, print it from the editor, or share it with other participants via a shareable. Web the process of getting prior approval from buckeye as to the appropriateness of a service or medication. However, this does not guarantee payment. Web buckeye community health plan’s preferred method for prior authorization requests. Our electronic.
Covermymeds Humana Prior Auth Form Form Resume Examples bX5aVMLOwW
Web prior authorization is a request made by you or your doctor to get wellcare by allwell's approval before receiving treatment. Providers need to send prior authorizations through. Pharmacy policies & forms coverage determinations and. Web buckeye health plan has reduced prior authorization requirements. During this process, we may request.
Buckeye group used Equation Group tools prior to ShadowBrokers
During this process, we may request. Inpatient prior authorization fax form (pdf) outpatient prior authorization fax form (pdf) cdms barcoded form disclosure (pdf). Prior authorization does not guarantee coverage. In response to is feedback, we have removed 22 services from our prior authorization inventory powerful. Pharmacy policies & forms coverage determinations and.
Download Your Modified Document, Export It To The Cloud, Print It From The Editor, Or Share It With Other Participants Via A Shareable.
Inpatient prior authorization fax form (pdf) outpatient prior authorization fax form (pdf) cdms barcoded form disclosure (pdf). We call this prior authorization. Web prior authorization is a request made by you or your doctor to get wellcare by allwell's approval before receiving treatment. However, this does not guarantee payment.
Include The Date To The Document With The Date Option.
Web buckeye community health plan’s preferred method for prior authorization requests. Web prior authorization request form save time and complete online covermymeds.com covermymeds provides real time approvals for select drugs, faster decisions and saves. Web buckeye health plan has reduced prior authorization requirements. If you don’t get approval, you.
Please Click View All Or Search By Generic Or Brand Name To Find The Correct Prior Authorization Fax Form For.
In response to is feedback, we have removed 22 services from our prior authorization inventory powerful. During this process, we may request. Our electronic prior authorization (epa) solution provides a safety net to ensure the. We require you to get approval from us before we agree to cover certain drugs.
Web Authorization Request Primary Procedure Code*Additional Procedure Codestart Date Or Admission Date*Diagnosis Code*.
Web prior authorization, step therapy, & quantity limitations; Providers need to send prior authorizations through. Pharmacy policies & forms coverage determinations and. Prior authorization does not guarantee coverage.