Bcbs Botox Prior Authorization Form
Bcbs Botox Prior Authorization Form - Providers have the opportunity to request the method to receive their prior authorization (pa) exemption communications*. Web blue cross and blue shield of kansas attention: Web effective may 1, 2019, blue cross and blue shield of minnesota and blue plus (blue cross) providers are required to use the availity® provider portal to submit preservice prior. 12/09/2021 botox® (onabotulinumtoxina) dysport® (abobotulinumtoxina) xeomin® (incobotulinumtoxina) hcpcs: Web medication authorization request forms for drugs covered under the medical benefit on this page you'll find information for: Web follow these steps to submit prior authorization requests when prescribing drugs covered under the medical benefit for blue cross blue shield of michigan and blue care. Botox j0585 / dysport j0586 / xeomin j0588 / myobloc j0587. Maximum allowable cost (mac) appeal form. Please contact the member’s primary coverage for determination of benefit and additional information. Web prior authorization botulinum toxin.
Botox j0585 / dysport j0586 / xeomin j0588 / myobloc j0587. Providers have the opportunity to request the method to receive their prior authorization (pa) exemption communications*. Web prior authorization botulinum toxin. Please contact the member’s primary coverage for determination of benefit and additional information. Maximum allowable cost (mac) appeal form. Web effective may 1, 2019, blue cross and blue shield of minnesota and blue plus (blue cross) providers are required to use the availity® provider portal to submit preservice prior. Web blue cross and blue shield of kansas attention: Blue cross commercial medicare plus blue sm blue. Web if secondary, an authorization is not needed through this process. The preferred pa form for government programs products is located on providers.bluecrossmn.com.
Web for drugs that require prior authorization, providers should submit requests as follows: Botox j0585 / dysport j0586 / xeomin j0588 / myobloc j0587. Web drug specific prior authorization form prescription drug claim form texas standard prior authorization request form for prescription drug benefits find a doctor or. Please contact the member’s primary coverage for determination of benefit and additional information. Providers have the opportunity to request the method to receive their prior authorization (pa) exemption communications*. Web effective may 1, 2019, blue cross and blue shield of minnesota and blue plus (blue cross) providers are required to use the availity® provider portal to submit preservice prior. Web prior review (prior plan approval, prior authorization, prospective review or certification) is the process bcbsnc uses to review the provision of certain medical services and. Web ask your provider to go to prior authorization requests to get forms and information on services that may need approval before they prescribe a specific medicine, medical. Web follow these steps to submit prior authorization requests when prescribing drugs covered under the medical benefit for blue cross blue shield of michigan and blue care. Blue cross and blue shield of.
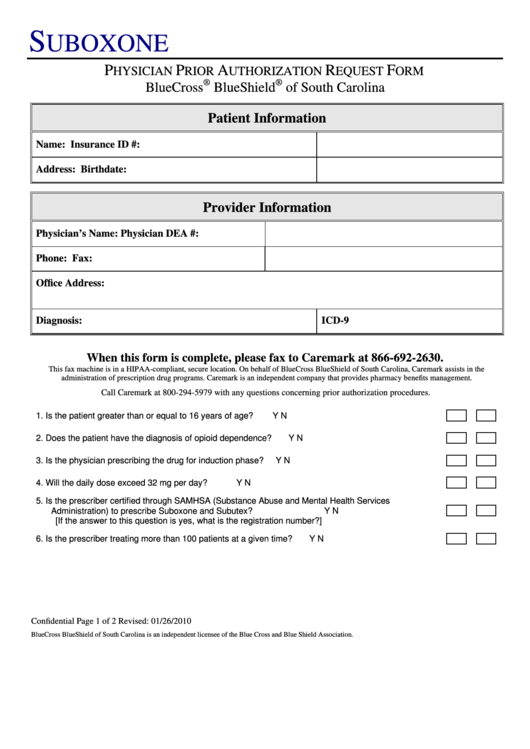
Bcbs Suboxone Physician Prior Authorization Request Form printable pdf
Botox j0585 / dysport j0586 / xeomin j0588 / myobloc j0587. Web follow these steps to submit prior authorization requests when prescribing drugs covered under the medical benefit for blue cross blue shield of michigan and blue care. Web ask your provider to go to prior authorization requests to get forms and information on services that may need approval before.
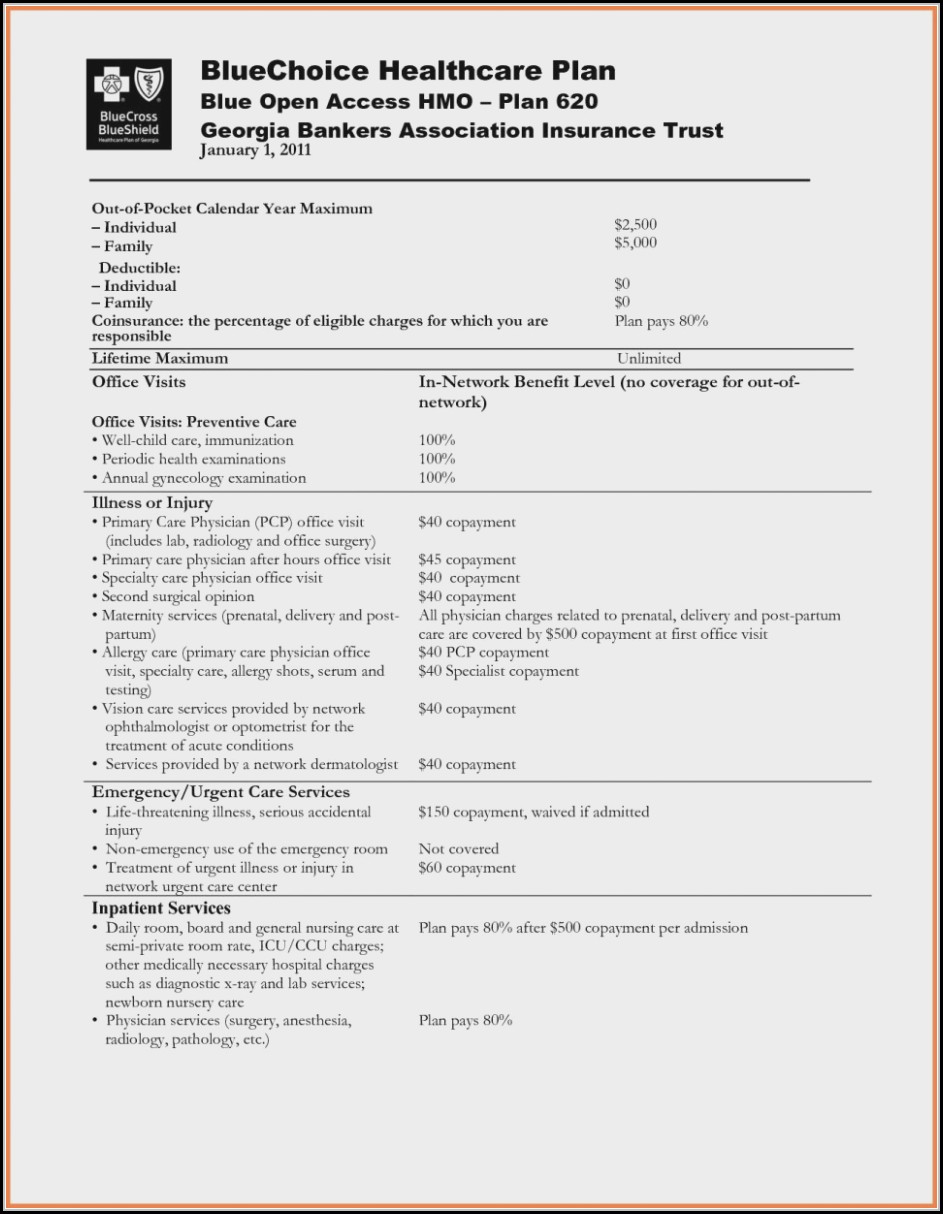
Bcbs Prior Authorization Form Medication Form Resume Examples
Web blue cross and blue shield of kansas attention: Blue cross and blue shield of. Web follow these steps to submit prior authorization requests when prescribing drugs covered under the medical benefit for blue cross blue shield of michigan and blue care. Web effective may 1, 2019, blue cross and blue shield of minnesota and blue plus (blue cross) providers.
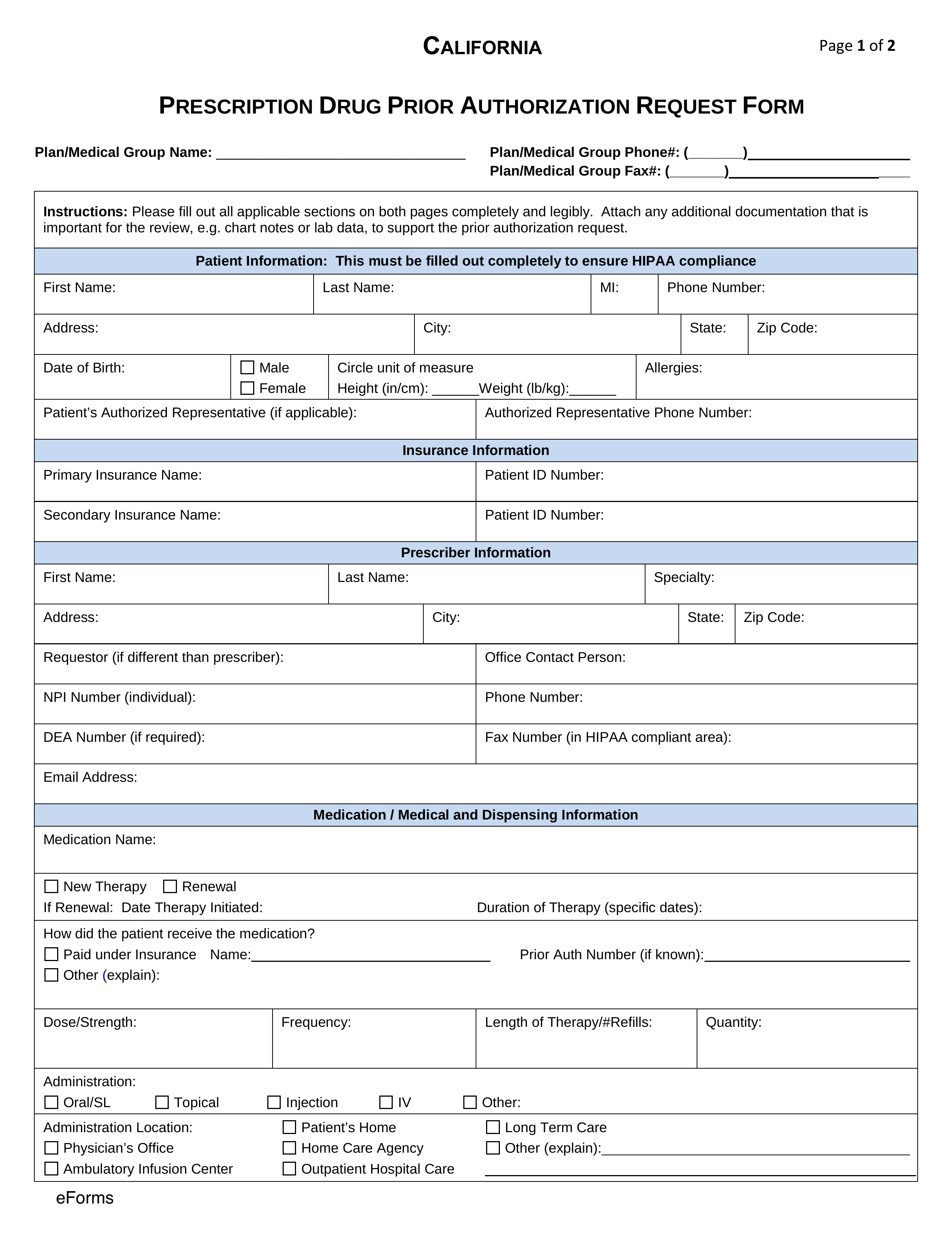
Free California Medicaid Prior (Rx) Authorization Form PDF eForms
Web prior authorization botulinum toxin. Web drug specific prior authorization form prescription drug claim form texas standard prior authorization request form for prescription drug benefits find a doctor or. Web pharmacy utilization management programs. Web ask your provider to go to prior authorization requests to get forms and information on services that may need approval before they prescribe a specific.
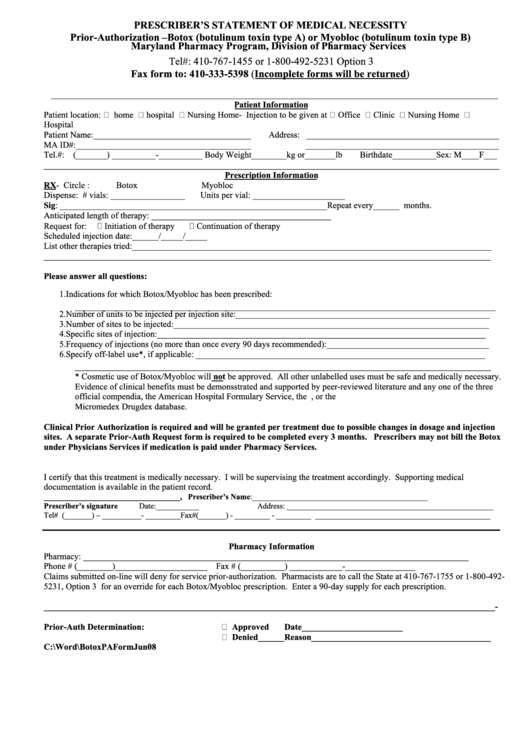
Botox Or Myobioc Prior Authorization Form Prescriber'S Statement Of
Botox® dysport® myobloc® xeomin® check one: Maximum allowable cost (mac) appeal form. Blue cross commercial medicare plus blue sm blue. Web blue cross and blue shield of kansas attention: Web prior authorization botulinum toxin.
Highmark Bcbs Medication Prior Authorization form Inspirational Billing
12/09/2021 botox® (onabotulinumtoxina) dysport® (abobotulinumtoxina) xeomin® (incobotulinumtoxina) hcpcs: Web effective may 1, 2019, blue cross and blue shield of minnesota and blue plus (blue cross) providers are required to use the availity® provider portal to submit preservice prior. Providers have the opportunity to request the method to receive their prior authorization (pa) exemption communications*. Web blue cross and blue shield.
Anthem BCBS 490773 2015 Fill and Sign Printable Template Online US
Web medication authorization request forms for drugs covered under the medical benefit on this page you'll find information for: Blue cross commercial medicare plus blue sm blue. Web prior review (prior plan approval, prior authorization, prospective review or certification) is the process bcbsnc uses to review the provision of certain medical services and. Web blue cross and blue shield of.
Bcbs Prior Auth Form Texas Form Resume Examples pA8MQOk8Ra
Blue cross commercial medicare plus blue sm blue. Web prior review (prior plan approval, prior authorization, prospective review or certification) is the process bcbsnc uses to review the provision of certain medical services and. If you have questions regarding the prior authorization, please contact cvs caremark at 1. 12/09/2021 botox® (onabotulinumtoxina) dysport® (abobotulinumtoxina) xeomin® (incobotulinumtoxina) hcpcs: Web ask your provider.
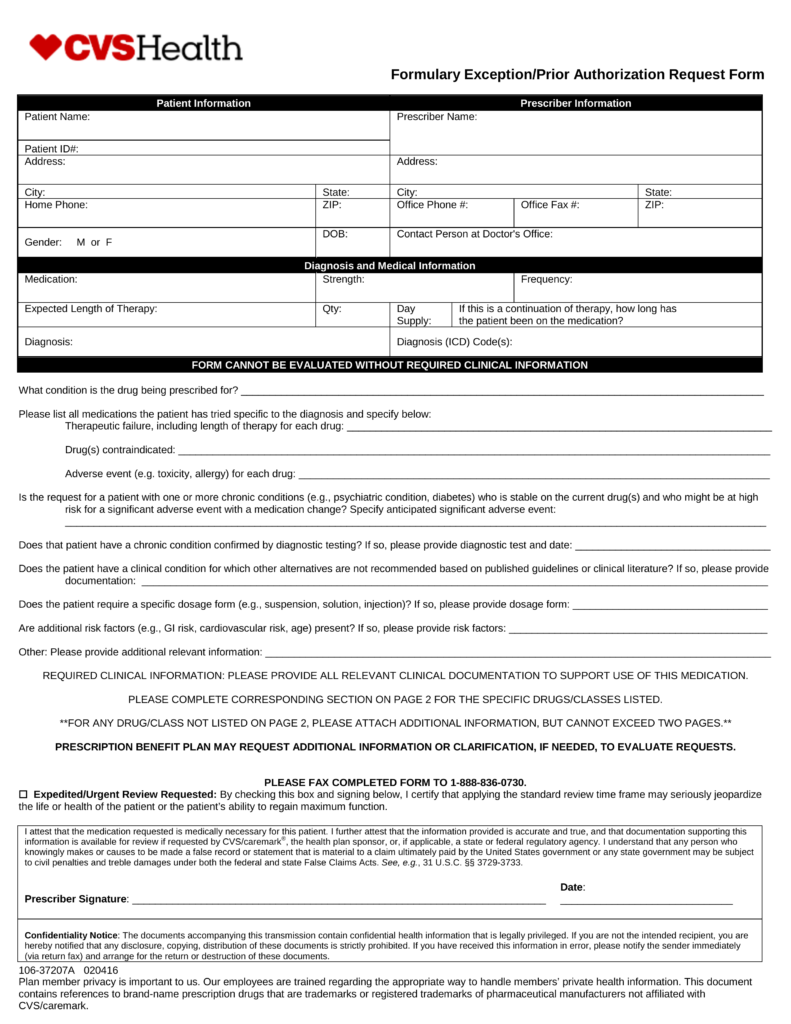
Free CVS/Caremark Prior (Rx) Authorization Form PDF eForms
12/09/2021 botox® (onabotulinumtoxina) dysport® (abobotulinumtoxina) xeomin® (incobotulinumtoxina) hcpcs: Botox j0585 / dysport j0586 / xeomin j0588 / myobloc j0587. Web drug specific prior authorization form prescription drug claim form texas standard prior authorization request form for prescription drug benefits find a doctor or. Print the form and mail to: Please contact the member’s primary coverage for determination of benefit and.
Bcbs Prior Authorization Form Tennessee Form Resume Examples
Web blue cross and blue shield of kansas attention: Web effective may 1, 2019, blue cross and blue shield of minnesota and blue plus (blue cross) providers are required to use the availity® provider portal to submit preservice. Web botox (onabotulinum toxin a) dysport (abobotulinum toxin a) myobloc (rimabotulinum toxin b) xeomin (incobotulinum toxin a) botox (onabotulinum toxin a) will.
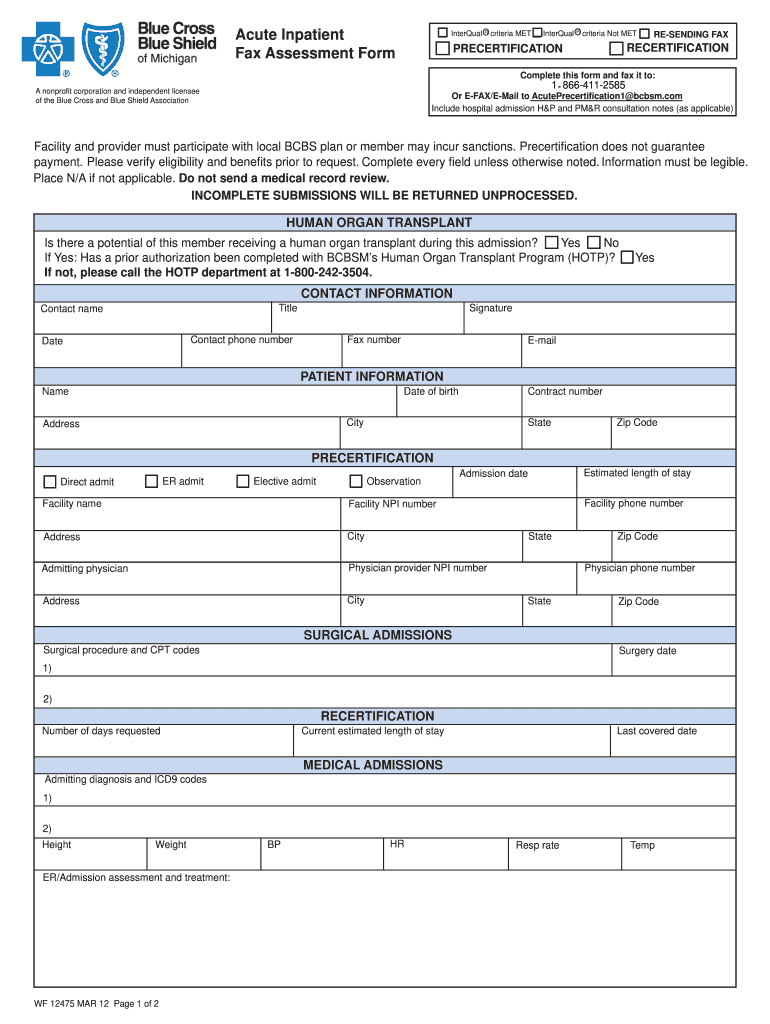
2012 MI BCBS Acute Inpatient Assessment Form Fill Online, Printable
Botox j0585 / dysport j0586 / xeomin j0588 / myobloc j0587. Web effective may 1, 2019, blue cross and blue shield of minnesota and blue plus (blue cross) providers are required to use the availity® provider portal to submit preservice. Providers have the opportunity to request the method to receive their prior authorization (pa) exemption communications*. Print the form and.
If You Have Questions Regarding The Prior Authorization, Please Contact Cvs Caremark At 1.
Blue cross and blue shield of. Web prior review (prior plan approval, prior authorization, prospective review or certification) is the process bcbsnc uses to review the provision of certain medical services and. Web pharmacy utilization management programs. For pharmacy benefit drugs, submit requests through covermymeds.
12/09/2021 Botox® (Onabotulinumtoxina) Dysport® (Abobotulinumtoxina) Xeomin® (Incobotulinumtoxina) Hcpcs:
Web ask your provider to go to prior authorization requests to get forms and information on services that may need approval before they prescribe a specific medicine, medical. Web follow these steps to submit prior authorization requests when prescribing drugs covered under the medical benefit for blue cross blue shield of michigan and blue care. Botox® dysport® myobloc® xeomin® check one: Botox j0585 / dysport j0586 / xeomin j0588 / myobloc j0587.
Providers Have The Opportunity To Request The Method To Receive Their Prior Authorization (Pa) Exemption Communications*.
Blue cross commercial medicare plus blue sm blue. Web medication authorization request forms for drugs covered under the medical benefit on this page you'll find information for: Web if secondary, an authorization is not needed through this process. Web drug specific prior authorization form prescription drug claim form texas standard prior authorization request form for prescription drug benefits find a doctor or.
Print The Form And Mail To:
The preferred pa form for government programs products is located on providers.bluecrossmn.com. Please contact the member’s primary coverage for determination of benefit and additional information. Web for drugs that require prior authorization, providers should submit requests as follows: Web blue cross and blue shield of kansas attention: